Introduction
One of the most significant obstacles to effective mental health care is establishing an objective measurement of patients’ progress in relation to the treatment regime or program they are receiving or are participating in. Perhaps the most challenging group with which to establish such objective measurements are those suffering from schizophrenia (which I shall henceforth refer to as metabolic dysperception, as it is more indicative of its mechanism and lacks stigma) and addictions. Errors of perception, depression and paranoia are some of the key symptoms experienced by these patients, yet it is often difficult for practitioners to agree on a definitive diagnosis as clinical interviews tend to be too short to ask patients the battery of questions required to make correct decisions (Kelm H, Hoffer A & Osmond H. 1981, p.1-2). It was to this end that Drs. Abram Hoffer and Humphry Osmond, in the early 1960s, created a test that lead to fewer errors in the diagnoses associated with metabolic dysperception and addictions, thus increasing efficiency and reducing the waste of medical resources and efforts. They named this test the HOD or Hoffer Osmond Diagnostic test (Hoffer A, Osmond H, 1961a). Unfortunately, few practitioners use the HOD test today. This paper explores some of the advantages that renewed use would bring to mental health, when to use it, and how to integrate it into a practice.
One particularly challenging obstacle clinicians face in determining the presence or absence of errors of perception lays in the one-on-one interview with the patient, who may be unwilling to reveal to a practitioner that their perceptual world is unstable due to self-consciousness about the stigma they believe it will place upon them. However, an instrument like the HOD test circumvents this self-consciousness due to it being a test that is read and answered by the patient on their own (Kelm H, Hoffer A & Osmond, 1981, p1-2). As a result, patients tend to reveal more honest information while taking the test (Kelm et al., 1981, p.2). During a patient consult, if the patient’s short-term memory is such that questions must be asked many times by the clinician, it can become tiresome for both parties and result in less information being elicited. The HOD test in conjunction with a clinical interview provides a much-needed clarification about how best to help patients with perceptual errors (Kelm H, Hoffer A, Osmond H, 1981, p.5).
If used regularly through the course of a patient’s treatment, the HOD can also function as a gauge of effectiveness of the therapy being employed (Hoffer, Kelm & Osmond, 1975). If the HOD scores consistently decrease during treatment, it is an indication that the therapy in question is working. If HOD scores begin to increase after being low, it is predictive of a relapse in chronic patients (Hoffer, 2009).
Although the HOD test is perhaps crude when compared to the Experiential World Inventory (EWI) test (Brisbee, Mullaly, 1980), it is shorter to administer, and in its form as a digital application (OrthoHOD Pro App) for smart phones and tablets, it also contains additional True/ False questions that can aid in understanding some of the orthomolecular nutrient dependencies that have been shown to exist within patients.
HOD Test Description
The original test is comprised of 145 True/ False questions covering visual, auditory, tactile, taste, time and olfactory perception, as well as thought and feeling disturbances. The answers that the patient labels as true are scored in several different scales. The questions in order are listed in the Appendix.
These scales include the following six categories with cut-off scores determining pathology for different age groups in Table 1.
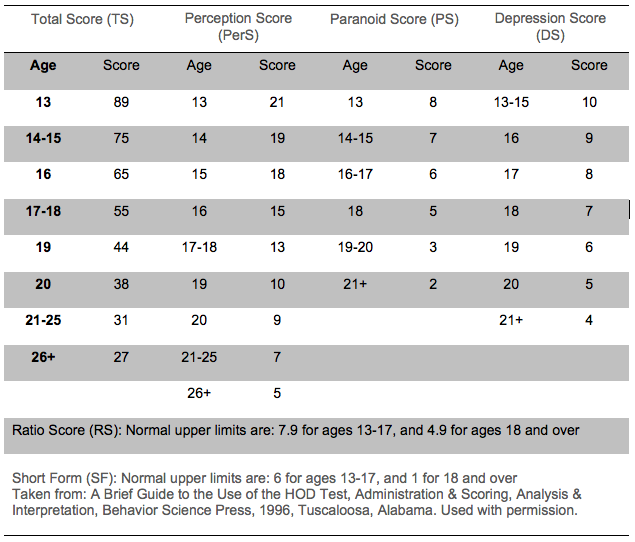
Perceptual Score (PerS) is based on 53 of the statements about perception and is a relative gauge of perceptual errors that a patient may be experiencing. Adults over 21 score above 7 when ill. (Hoffer, Osmond 1961a, 1962a), (Kelm, Hoffer & Osmond, 1981)Total Score (TS) is the most comprehensive of the scores and gives an overall measure of the patient’s present condition. It functions as a gross classification of either having perceptual errors or not, based on age related cut-off values that had been established via extensive test trials performed in Saskatchewan Mental Hospitals and in private practice (Hoffer, Kelm & Osmond, 1975). When an adult over the age of 21 scores over 30 it indicates metabolic dysperception (Kelm, Hoffer & Osmond, 1981). It is calculated as a weighted score of different groups of the above-mentioned perceptual categories.
Paranoid Score (PS) measures how suspicious a patient currently is, and is comprised of 15 statements. This is generally indicative of how well a patient is able to maintain inter-personal relationships (Hoffer, Kelm & Osmond, 1975). Scores in excess of 2 in adults over age 21 indicate illness.
Depression Score (DS) includes 18 statements that determine both the affective state (mood) as well as the risk of suicide that a patient might have. If a DS of over 4 occurs, the patient is depressed (Hoffer, Kelm & Osmond, 1975).
Ratio Score (RS) is based on the following formula: RS = TS/DS, when DS = 0, RS = TS x 2. This score helps to make a sharper distinction between metabolic dysperception patients and others. It is, however, used in conjunction with the total and depression scores as opposed to a stand-alone score as normal patients can have similar ratio scores even though they do not suffer from perceptual errors (Hoffer, Kelm 1970).
Short Form (SF) is composed of the 17 statements that statistical analyses confirmed to be the most important in differentiating dysperceptive from non-dysperceptive patients. It was found to act as an emergency test for existing psychiatric patients when there was insufficient time to administer the full test (Kelm, Callbeck & Hoffer, 1967). However, it is important not to rely on this score by itself as a means of diagnosing metabolic dysperception.
These scores enable a consistent and reliable assessment of mentally ill patients to be performed on a regular basis, with minimal time requirements. From an efficiency point of view, this is highly desirable as mental health resources are often stretched to their limits in many societies, ours notwithstanding (Krieg et al. 2016).
Administration of the HOD Test
In the past, when administering the test to patients in a psychiatric ward, it was important to explain the test to the patient in the following manner:
“This is a very broad test covering all the possibilities from quite sick to only minor nervousness. There are some pretty
wild questions on the test – don’t let that bother you. If you have a particular pattern on the test, there is something that can be done about it easily” (Ward, 1967).
While this explanation was functional in the 1960s, a better strategy might be to take the patient’s medical/ physical history, then ask if they would mind having their stress levels measured and explaining the test as follows:
“This test is not a test of IQ or personality but it will help to give us insight into any nutritional dependencies you may be experiencing that will effect your abilities of perception. Although some of the questions are slightly strange, there are no wrong answers. Make sure to answer all of the questions based on how you are feeling right now. This will help us to determine the right nutrients to give you, in order to correct any dependencies”.
The advantage of this approach is that as the test takes between 10 and 15 minutes, it will give the practitioner some time to ponder the patient’s history, and the corresponding approach to take vis-à-vis treatment.
When to Use the HOD Test
During a patient interview, the clinician will usually be able to determine when the HOD test will be most appropriate to administer based on the following criteria:
- When a patient gives a vague description of medical issues such as fatigue or tiredness
- When a patient gives an inconsistent description of body pains
- When the patient’s pains are non-mechanical
- When a patient complains of depression, insomnia, anxiety and/or admits to being stressed
- When a patient specifically wants an alternative to pharmaceutical medications for depression
- When a patient gives a confusing or inconsistent history
Interpreting the HOD Test
The test makes clear the distinction between those patients who are experiencing high levels of perceptual errors and those who are not (Hoffer A, Kelm H & Osmond H. 1975, p.12-17). High levels of perceptual errors, paranoia and depression are indicative of a metabolic dysperception type of illness. As has been demonstrated by abundant research, psychoanalysis is not effective on those whose perceptual world is unstable (Hoffer, 2005, p.34).
Some other relationships within the test are also worth mentioning. Certain combinations of questions have been shown to give the practitioner useful emergency information concerning the status of the tested patient when:
- Item 76 is answered true, the patient has insight into the fact that they are sick.
- Items 106 and 107 are answered true, severe depression is suggested,
- Items 131 and 145 are answered true, failure of self-perception is suggested.
- Item 143 is answered true, the patient believes that others hate him/her.
- Item 76 is answered false, and 106, 107, 131, 143 and 145 are answered true, the patient has a high risk of suicide.
- Item 76 is answered false, 143 is true and there is a Paranoid Score (PS) of 8 or higher, violence or homicidal thoughts should be suspected and discussed.
The HOD test also has a way of telling if the subject may be fabricating their answers (Hoffer et al. 1975). If items 82-101 have been marked false, the subject has not been honest (Hoffer, Kelm & Osmond, 1975, p.26). Whether this dishonesty was deliberate or not is difficult to say, but should this occur, the test will be ineffective. The scoring mechanisms are listed and explained in the Appendix.
Other Potential Uses of the HOD Test
Although Drs. Hoffer and Osmond touched only briefly on addictions (Hoffer, Kelm & Osmond, 1975, p. 49-50), the test can also be used to evaluate progress in addiction treatment. The reason for this stems from the perception- altering nature of many substances that cause addiction (alcohol, opiates, etc.). The cut-off TS score for adults over the age of 26 of normal cognition is 27 (Kelm et al., 1981). Any scores below this are indications that the patient is less likely to be suffering from metabolic dysperception. Osmond demonstrated that a HOD score of 80 would be elicited in a person of normal cognition with doses of LSD-25 of 60-80 mcg, 200-300 mg of mescaline or even someone suffering with a fever of 102°F or 39°C (Hoffer et al. 1975, p.50). Peters (1970) demonstrated that HOD scores in novice cannabis smokers ranged from 50-60, while LSD caused scores of between 70-90, and amphetamine users scored up to 150.
All substances that alter cognition could potentially have their impact measured via HOD scores. This would be very valuable if used in the treatment of substance abuse, as per capita medical costs in 2002 for complications arising from substance use and misuse in Canada were $1,267 with $463 attributed to alcohol, and $262 to illegal drugs (Rehm et al. 2002). The portions of these costs associated with medical care were 22% of the totals (Rehm et al. 2002). Using the HOD test in addiction evaluation and treatment can have two potential benefits. First, it can gauge patient progress while in treatment and second, it is able to spot metabolic dysperception in patients who have been abstinent from substances yet have been undiagnosed with this condition, or those for whom a relapse is likely (Hoffer et al. 1975, p.51).
As medical cannabis comes into greater use as a therapy, the HOD can also be used as a screening tool to determine the suitability of this substance (Hoffer, Kelm & Osmond, 1975, p.52). In a certain section of the population, cannabis has been shown to cause psychotic breaks (Korver et al. 2010). This cross section of people, most likely have an undiagnosed psychiatric disorder. Until now, there has been no way to quickly determine the suitability of this medication in a primary care practice (Hoffer, Kelm & Osmond, 1975, p.52).
Another benefit to this test is its versatility in being administered by a wide range of health practitioners (Hoffer et al. 1975, p.21). Sometimes it is difficult to know when to refer a patient to another professional to optimize a patient’s care. This test helps to better define these parameters, and may help to foster better interdisciplinary cooperation. It can also help to prevent patients from being misdiagnosed.
Conclusions
The HOD test provides an additional, effective tool for practitioners from many branches of medicine. Due to its ease of use (OrthoHOD Pro App for smartphone and tablet), relative simplicity and amount of clinical information generated, it would improve diagnostic efficiency, prevent diagnostic errors and improve patient care, while ultimately saving taxpayers’ money. As medical cannabis and hallucinogen-assisted psychotherapies gradually become more used in medicine, the HOD test could give patients and practitioners an extra margin of safety in their judicious use.
Competing Interests
Alexander Audette is the developer and Richard Johnson is the advising developer of the OrthoHOD Pro App for smart phones and tablets; Dr. Anello has no competing interests.
References
Bisbee C, Mullaly R (1980), Therapeutic Uses Of The Experiential World Inventory, Orthomolecular Psychiatry, Vol. 9, No. 1, Pp. 11 -20.
Hoffer A (2005), Adventures in Psychiatry: The Scientific Memoirs of Dr. Abram Hoffer, Caledon, ON KOS Publishing.
Hoffer A (2009), Orthomolecular Treatment of Schizophrenia, Journal of Orthomolecular Medicine, Vol. 24, No. 3 & 4.
Hoffer A, Kelm H, Osmond H (1975). Clinical and Other Uses of the Hoffer-Osmond Diagnostic Test. Huntington, NY: Robert E. Krieger Publishing Company.
Hoffer A, Osmond H (1961a). A card sorting test helpful in making psychiatric diagnosis., Journal of Neuropsychiatry, 2, 306-330.
Hoffer A, Osmond H (1962a). The association between schizophrenia and two objective tests., The Canadian Medical Association Journal, 87, 641-646.
Hoffer A, Kelm H (1970). Inappropriate mood and schizophrenia. Schizophrenia, 2, 116-118.
Kelm H, Hoffer A, Osmond H (1981). Hoffer-Osmond Diagnostic Test Manual (Revised Edition). Tuscaloosa, AB: Behavior Science Press.
Kelm H, Callbeck MJ, Hoffer A, (1967). A short form of the Hoffer-Osmond Diagnostic Test., International Journal of Neuropsychiatry, 3, 489.
Nikie Korver , Dorien H. Nieman, Hiske E. Becker, J. Reinaud van de Fliert, Peter, H. Dingemans, Lieuwe de Haan, Mark Spiering, Nicole Schmitz, Don H. Linszen,(2010). Symptomatology and neuropsychological functioning in cannabis using subjects at ultra-high risk for developing psychosis and healthy controls., Australian and New Zealand Journal of Psychiatry; 44:230–236.
Krieg C, Hudon C, Chouinard MC, Dufour I (2016) Individual predictors of frequent emergency department use: a scoping review. BMC Health Serv Res;16(1):594.
Peters G, A study of psychedelic drug users. Schizophrenia, 1970, 2, 103-108.
Rehm J, Gnam W, Popova S, Baliunas D, Brochu S, Fischer B, Patra J, Sarnocinska-Hart A, Taylor B, (2007), The Costs of Alcohol, Illegal Drugs, and Tobacco in Canada, 2002. Journal of Studies on Alcohol and Drugs;68(6):886-95.
Ward J L. (1967), Treatment of neurotics and schizophrenics using clinical and HOD criteria. Journal of Schizophrenia, 1, 140-149.
Appendix
HOD Questions (in order):
True or false is to be indicated for each statement.
(Visual Perception)
- People’s faces sometimes pulsate as I watch them.
- People’s faces seem to change in size as I watch them.
- People’s eyes seem very piercing and frightening.
- People watch me a lot more than they used to.
- People watch me all the time.
- I feel rays of energy upon me.
- Most people have halos (areas of brightness) around their heads.
- Sometimes I have visions of people when I close my eyes.
- Sometimes I have visions of people during the day when my eyes are open.
- Sometimes I have visions of animals or scenes.
- Sometimes I have visions of God or of Christ.
- Sometimes the world seems unreal.
- Sometimes I feel very unreal.
- When I look at things like tables and chairs they seem strange.
- When I look at people they seem strange.
- Often when I look at people they seem to be like someone else
- Now and then when I look in the mirror my face changes and seems different.
- My body now and then seems to be altered – too big or too small, out of proportion.
- Sometimes the world becomes very bright as I look at it.
- Sometimes the world becomes very dim as I look at it.
- Sometimes when I read the words begin to look funny – they move around or grow faint.
- Sometimes when I watch TV the picture looks very strange.
- Sometimes I feel there is a fog or mist shutting me away from the world.
- Sometimes objects pulsate when I look at them.
- Pictures appear to be alive and to breathe.
- I often see sparks or spots of light floating before me.
- My hands or feet sometimes seem much too large for me.
- I sometimes feel that I have left my body.
- I often feel I have left my body.
(Auditory Perception)
- My sense of hearing is now more sensitive than it ever has been.
- I now have more trouble hearing people.
- I often have singing noises in my ears.
- I often hear or have heard voices.
- I often hear or have heard voices talking about or to me.
- I have often felt that there was another voice in my head.
- I have often heard strange sounds, e.g. laughing, which frighten me.
- I have heard voices coming from the radio, television, or tape recorders talking about me.
(Tactile Perception)
- My sense of touch has now become very keen.
- I sometimes have sensations of crawly things under my skin.
- I sometimes feel rays of electricity shooting through me.
- Some of my organs feel dead.
- I sometimes feel my stomach is dead.
- I sometimes feel my bowels are dead.
- I sometimes feel I am being pinched by unseen things.
- I now have trouble feeling hot or cold things.
- I sometimes feel strange vibrations shivering through me.
(Taste Perception)
- Some foods that never tasted funny before do so now.
- I can taste bitter things in some foods like poison.
- Foods taste flat and lifeless.
- I have more difficulty tasting foods now.
- Water now has funny tastes.
(Time Perception)
- I can no longer tell how much time has gone by.
- The days seem to go by very slowly.
- Some days move by so quickly it seems only minutes have gone by.
- I have much more trouble keeping appointments.
- I have much more trouble getting my work done on time.
(Olfactory Perception)
- Things smell very funny now.
- My body odor is much more noticeable than it once was.
- My body odor is much more unpleasant now.
- I sweat much more now than when I used to.
- I can no longer smell perfumes as well as I used to.
- Foods smell funny now.
(Thought)
- At times my mind goes blank.
- At times my ideas disappear for a few moments and then reappear.
- I am bothered by very disturbing ideas.
- My mind is racing away from me.
- At times I am aware of people talking about me.
- There are some people trying to do me harm.
- There is some plot against me.
- I have a mission in life given to me by God.
- At times some other people can read my mind.
- I can read other people’s minds.
- At times when I come into a new situation, I feel strongly the situation is a repeat of one that happened before.
- I now become easily confused.
- I am now much more forgetful.
- I am now sick.
- I cannot make up my mind about things that before did not trouble me.
- My thinking gets all mixed up when I have to act.
- I very often get directions wrong.
- Strange people or places frighten me.
- People are watching me.
- A cow is like a horse because they both live on a farm, not because they are both animals.
- A cow is like a horse because they are animals, not because they both live on a farm.
- A chair is like a table because they have four legs, not because they are usually used together.
- A chair is like a table because they are usually used together rather than because they both have four legs.
- A dress is like a glove because they belong to women rather than because they are articles of clothing.
- A dress is like a glove because they are articles of clothing rather than because women own them.
- A pen is like a pencil because they are like sticks, rather than because they are used for writing.
- A pen is like a pencil because they are both used for writing rather than because they both are like sticks.
- An orange is like a banana because they both have skins rather than because they are fruit.
- An orange is like a banana because they are fruit, not because they both have skins.
- An axe is like as saw because they have handles, rather than because they are tools.
- An axe is like a saw because they are tools, rather than because they have handles.
- The eye is like the ear because they are on the head rather than because they are sense organs.
- The eye is like the ear because they are sense organs rather than because they are on the head.
- Air is like water because they are both cold rather than because they are needed for life.
- Air is like water because they are needed for life rather than because they are both cold.
- Praise is like punishment because they both start with the letter P rather than because they are given to people.
- Praise is like punishment because they are both given to people rather than because they start with the letter P.
- A fly is like a tree because they both require humans rather than because they are living things.
- A fly is like a tree because they are both living things rather than because they both require humans.
(Feelings)
- I very often am very tired
- I very often suffer from severe nervous exhaustion.
- I very often have great difficulty falling asleep at night.
- I usually feel alone and sad at a party.
- I usually feel miserable and blue.
- Life seems entirely hopeless.
- I am very painfully shy.
- I am often misunderstood by people.
- I have to be on my guard with friends.
- Very often friends irritate me.
- My family irritates me very much.
- I am often very shaky.
- I am constantly keyed up and jittery.
- Sudden noises make me jump or shake badly.
- I often become scared of sudden movements or noises at night.
- My hands or feet sometimes feel far away.
- My hands or feet often look very small now.
- Cars seem to move very quickly now. I can’t be sure where they are.
- When I am driving in a car objects and people change shape very quickly. They didn’t used to.
- I often hear my thoughts inside my head.
- I often hear my own thoughts outside my head.
- I hear my own thoughts as clearly as if they were my own voice.
- My bones often feel soft.
- Cigarettes taste strange now.
- Other people’s cigarette smoke smells strange – like a gas.
- The world has become timeless for me.
- Time seems to have changed recently, but I am not sure how.
- Other people smell strange.
- People look as if they were dead now.
- I feel as if I am dead.
- People are often envious of me.
- Many people know that I have a mission in life.
- People interfere with my body to harm me.
- People interfere with my body to help me.
- People interfere with my mind to harm me.
- People interfere with my mind to help me.
- I know that most people expect a great deal of me.
- Lately I often get frightened when driving myself in a car.
- I get more frightened now when I am driven in a car by others.
- I don’t like meeting people – you can’t trust anyone now.
- More people admire me now than ever before.
- Most people hate me.
- I find that past, present and future seem all muddled up.
- I am not sure who I am.
Scoring Mechanisms:
Total Score: 26 items (if scored true) are given a weight of 5 points: items – 1, 2, 14, 34, 36, 37, 44, 52, 57, 68, 72, 117, 118, 119, 120, 121, 122, 128, 129, 130, 134, 136, 139, 141, 143, 145.
4 items (if scored true) are given a weight of 2 points: items – 82, 86, 92, 100.
10 statements are not scored: items – 83, 85, 87, 89, 91, 93, 95, 97, 99, 101.
Remaining 105 statements (if scored true) are given 1 point each. (The total possible score is 243).
Perceptual Score Items (PerS): (each item scored TRUE receives 1 point)
Questions: 1, 2, 4, 5, 7, 9, 10, 11, 12, 13, 14, 15, 17, 18, 21, 23, 24, 27, 28, 29, 33, 34, 35, 36, 37, 39, 40, 41, 42, 43, 44, 48, 51, 52, 54, 57, 62, 117, 118, 119, 120, 121, 122, 123, 124, 125, 126, 127, 128, 129, 130, 131, 144. (total possible score is 53)
Paranoid Score (PS): (each item scored TRUE receives 1 point)
Questions: 4, 5, 34, 67, 68, 69, 81, 132, 134, 135, 136, 137, 141, 142, 143. (total possible score is 15)
Depression Score (DS): (each item scored TRUE receives 1 point)
Questions: 20, 31, 49, 53, 56, 77, 78, 102, 103, 104, 105, 106, 107, 111, 112, 113, 114, 115. (Total possible score is 18)
Short Form (SF): (each item scored TRUE receives 1 point)
Questions: 3, 5, 10, 16, 28, 33, 34, 35, 37, 68, 69, 121, 122, 123, 132, 136, 141. (Total possible score is 17)
Ratio Score (RS): TS/DS=RS (if DS=0, TSx2=RS) (total possible score is 452)


