Introduction
In recent years psychological factors associated to different conditions have taken a prominent position in health sciences. The raise of mental (psychological/psychiatric) conditions and their consequences have made clear the need for more comprehensive therapeutic approaches. This is particularly important in face of the aggressive actions suffered by individuals with psychopathology, as well as the aggressive behaviors they tend to show, putting them in a difficult position. Human aggression and violence are an unfortunate global phenomenon with substantial costs to society (Siever, 2008). Therefore, legal and social aspects of violence, aggression and crime get the greatest attention from society, government and the media. While the foundations of human aggression are clearly multifactorial, including political, socioeconomic, cultural, medical, and psychological factors, it is also clear that some forms of pathological aggression, such as impulsive aggression (which occurs in the context of emotional arousal and provocation), have an underlying neurobiology/ biochemical root (Siever, 2008). However, deleterious effects of deficient nutritional intake on the neurobiological/biochemical substrates of behavior directly related to criminal activities are hardly addressed. In the last three decades, evidence on the association between dietary status and (deviant) behavior has increased (Zaalberg, Nijman, Bulten, Stroosma, & van der Staak, 2009). Neurobiological experiments have shown that many of the same neurochemical and anatomical systems are activated during aggressive behavior in humans and animals, even though the specific behavioral outputs can differ greatly (Nelson & Trainor, 2007). Still a number of factors have limited the benefits which a neurobiological perspective on violence might bring (Umhau, Trandem, Shah, & George, 2012).
.
Psychopathology
Irrespectively of their professional and theoretical background, therapists should be aware of the diverse manifestations of psychopathology (Oltsmanns & Castonguay, 2013). In order to conceptualize what a psychopathologic disorder is we first cite the most recent definition from the American Psychiatric Association (APA) in the Diagnostic and Statistical Manual of Mental Disorders 5th Edition: “A mental disorder is a syndrome characterized by clinically significant disturbance in an individual’s cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning. Mental disorders are usually associated with significant distress or disability in social, occupational, or other important activities. An expectable or culturally approved response to a common stressor or loss, such as the death of a loved one, is not a mental disorder. Socially deviant behavior (e.g., political, religious, or sexual) and conflicts that are primarily between the individual and society are not mental disorders unless the deviance or conflict results from a dysfunction in the individual, as described above (APA, 2013, p. 20).”
On the other hand, Wakefield (2010) developed another view coining the term “harmful dysfunction”. According to this position a disorder is a “harmful dysfunction” in which “harmful” is a value-based term that refers to conditions judged negative by sociocultural standards, and “dysfunction” is a scientific factual term, denoting failure of biologically designed functioning. In modern science, “dysfunction,” the author argues, is ultimately anchored in evolutionary biology and refers to the failure of an internal mechanism to perform one of its naturally selected functions.
Interestingly, both definitions acknowledge the inclusion of cognitive, behavioral and biological aspects of psychopathology. However, it is essential to understand that when talking about the biological factors associated to psychopathology and aggression, the energetic aspects must be taken into account. Therefore, nutritional intake, as the energy producing elements, should be investigated and included into understanding and treating these conditions.
.
Aggressive Behavior
Aggressive behavior is prevalent in social interactions in both humans and animals, and is highly heterogeneous in its origins and manifestations ranging from verbal insults to full-blown physical violence (Krämer, Riba, Ritcher, & Münte, 2011). In addition, Nelson and Trainor (2007), indicate that mental disorders such as post-traumatic stress disorder (PTSD), intermittent explosive disorder, irritable aggression and depression-linked aggression are associated with increased autonomic arousal, which can contribute to sudden and uncontrolled reactive aggression.
In 2000, there were an estimated 520, 000 homicides worldwide, for an overall age-adjusted rate of 8.8 per 100,000 population (Krug et al., 2002). This is an alarming number of deaths due to violent behavior. In the United States estimates of the cost of violence reach 3.3% of the gross domestic product (Waters et al., 2004). It has definitely become a public health problem. But, how is violence defined? The World Health Organization (WHO) defines violence as: “the intentional use of physical force or power, threatened or actual, against oneself, another person, or against a group or community, that either results in or has a high likelihood of resulting in injury, death, psychological harm, maldevelopment or deprivation” (Krug et al., 2002). Even though this definition reflects the physical, psychological, social, and economical implications of violence, it primarily focuses on the violent act. As a result, it directs diverse interventions in legal terms which reinforce the use of governmental/political strategies such as strengthening the tools for law enforcement, making stricter laws, and promote a better education. The first two, ought to serve as deterrents of violent and criminal behavior whereas education strives to instill the internalization of adequate social interactions and healthy conflict resolution.
These interventions, though useful, respond directly to the definition exposed above which focuses on violence as the initial step in a process that yields great social consequences. However, in our optic violence should be viewed in terms of deeper interaction that would include the neurobiological substrates of behavior. With all this being said, in our position, violence and aggression should be contextualized as the product of a dynamic interrelation between psychological, social and neurobiological factors which should include nutrition (vitamins and minerals) as an important variable in the biochemical genesis of violent behavioral manifestations.
.
Psychopathology and Aggression: The Two Sides of a Coin
Even though aggression and violence in general have increased significantly, they are also typical traits seen in persons with several neurocognitive and psychological/psychiatric disorders. Furthermore, the manifestations of violence have a biological/biochemical basis, reflected in the development of aggression and its regulatory neural mechanisms (Mercadillo & Arias, 2011). According to McCabe and Shaw (2010), recent research has identified specific neurotransmitters and receptor sites implicated in a variety of functions associated with cognition, emotion and behavior.
According to Pliszka (2016) humans typically engage in diverse maladaptive behaviors that are harmful to others, violate societal standards, and can even involve consuming substances to the point of developing addictions. The author points out that a number of studies show that ADHD in early childhood, especially when combined with learning disability and family adversity is highly predictive of delinquent behavior during teenage years.
According to a research conducted by Lober, Brinthaupt and Green (1988) cited in Pliszka (2016) criminal offenders in a sample of adolescents 1.7% of adolescents without ADHD or conduct disorders were multiple offenders; 3.4% has ADHD without conduct disorders; 20.7% did show conduct disorders but no history of ADHD were multiple offenders, and 30.8% of multiple offenders had comorbidity of conduct disorders and ADHD.
In another example, in relation to the various symptoms present in personality disorders, it is important to be aware of the emotional regulation and the capacity for emotional experience of the individual, as it happens in Borderline Personality disorder (BPD) which is characterized by difficulty of emotional regulation (Magnativa, Powers, Barber, & Oltsmanns, 2013). Moreover personality psychopathology is strongly associated with detrimental effects in family and social interactions; therefore actions are to be taken in a violent relationship, either as victim or perpetrator (Magnativa, Powers, Barber & Oltsmanns, 2013). Personality psychopathology is strongly associated with disturbing family and social interactions; therefore actions are to be taken is in a violent relationship, either as victim or perpetrator (Magnativa, Powers, Barber & Oltsmanns, 2013).
In contrast, a research conducted by Hiday, Swartz, Swanson, Borum and Wagner, (1999) showed that individuals with severe psychiatric disorders (schizophrenia, schizoaffective disorder, affective disorders with psychotic features) that were not taking medication were found to be 2.7 times more likely to be the victims of a violent crime (assault, rape, or mugging) than the general population.
These examples show the vulnerability of persons, especially young individuals with these conditions. Studies indicate that even they are more prone to aggressive behaviors, are also more vulnerable to suffer or be victims of aggression. However, the clinical and investigative questions to understand and treat these individuals should take into account, in addition to the psychological and social factors, the energetic and nutritional aspects that make them so vulnerable. For example, when the organism is under significant levels of stress, it requires greater amounts of nutrients to cope with the need of energy required by the body. If, in addition, the individual has a neurophysiological/neurochemical vulnerability that is manifested through mood changes and neurocognitive deficits, it will require even greater quantities of nutrients to replenish and rebalance the energetic depletion.
According to Silver and Yudofsky (1997) violent and explosive behavior has been associated with neuropsychiatric disorders with episodes ranging in severity from irritability to outbursts resulting in damage to property or even assaults on others; therefore Multidisciplinary and multifactorial collaborative approach in treating aggressive behavior is necessary in most cases (Silver & Yudofsky, 1997).
Numerous researchers have explored the relation between nutritional problems and maladaptative behaviors, suggesting there is a relationship between them (Rodríguez, González & Miranda, 2008). According to Benton (2007), there is a suggestion considering that food intolerance, additives, sugar intake, a low micro-nutrient intake, fatty acid deficiency and a tendency to develop hypoglycemia predispose to violence, anti-social behavior and crime. In addition, Davidson and Kaplan (2012), evaluated the relation between nutrient intake and psychiatric functioning in adults with confirmed mood disorders. The results of their study showed an association between higher levels of nutrient intakes and better mental health.
On the other hand, Rucklidge, Harrison and Johnstone (2011), exposed that little research has studied how micronutrients (minerals and vitamins) affect cognitive functioning, despite preliminary studies showing they may improve psychiatric functioning. However, as previously mentioned, during the decades, a growing body of evidence has exposed the association between dietary status and deviant behavior (Zaalberg, Nijman, Bulten, Stroosma, & van der Staak, 2009). Mendes et al. (2009), indicated that it is fundamentally important to study the risk and protective factors of the development of aggressive behavior. They point out that the first investigations about this topic focused on the social and environmental aspects of aggressiveness citing as examples Buss and Shackelford (1997), and Okami and Shackelford (2001). In addition, the authors expressed that with the elucidation of the biological/biochemical mechanisms (genetic and neurophysiological) implicated in aggressive behavior by means of recent studies in neuroscience, it has been concluded that social and environmental factors are not exclusive to explain the development of aggressive and antisocial behavior. They concluded that what in fact happens is an interaction between biological and social-environmental factors in the modulation of violent behavior.
As stated above, aggression and violence in general are also typical traits seen in persons with several neurocognitive and psychological/psychiatric disorders. The psychological and neurobiological deficits in these disorders make the person more prone to engage in violent acts. However, even though most would agree that good nutrition is fundamental for good physical health, the role of nutrition in maintaining good mental health has not been properly addressed in spite of the fact that the importance of micronutrients (i.e., vitamins and minerals) for normal brain function is well established by decades of scientific research (Kaplan et al., 2004).
.
The Brain and Micronutrients
According to Watson and Breedlove (2012), the brain must monitor and regulate a wide range of nutrients: 20 amino acids, several fatty acids, about 15 vitamins, and a variety of minerals, carbohydrates for energy, among others. They add that no animal can afford to run out of energy or nutrients, and therefore we need a system to anticipate future needs and keep an adequate reserve.
On the other hand, Keunen, van Elburg, van Bel and Benders (2015), have indicated that in animal models, malnutrition during a vulnerable period of brain development leads to a decrease in brain cells, myelin production, and number of synapses, in addition to alterations in neurotransmitter systems. Neuronal communication is possible by the release of chemical messengers called neurotransmitters (Grader & Bateman, 2017) which require of adequate nutritional intake to be synthesized. Also, developmental studies suggest that in early development a poor nutritional status can lead to behavioral consequences (Zaalberg, Nijman, Bulten, Stroosma, & van der Staak, 2009). In addition, Higgins and George (2009), establish that the human brain is an electrical organ which ineffectiveness in maintaining its functioning is common. Therefore, they explain that a portion of the individual’s daily caloric intake is utilized to maintain its operations. These authors also indicate that during day and night, the brain maintaining and discharging action potentials. Mozaffarian (2012), explains that nerves send electrical signals along thousands of miles of brain and body pathways, tissues formulate protein and fatty acid chemical messengers that go from organ to organ, issuing the orders that orchestrate and sustain life. Higgins and George (2009), add that the brain represents a 2% of body weight, receiving 15% of the cardiac output, 20% of body oxygen consumption, and 25% of total glucose utilization. Therefore, they explain that energy consumption required for the brain to survive is 0.1 calories per minute.
On the other hand Zimmermann (2001), indicates that about 45 essential micronutrients are indispensable for life and must be supplied through the diet because they cannot be synthesized in the human body. These essential vitamins and minerals are often called micronutrients because your body needs only small amounts of them (Mozaffarian, 2012). This complicated multi-pathway metabolic processes will entail the use of many nutrient cofactors to sustain the necessary enzymatic activity to perform such a complex task.
To perform a wide array of functions ranging from muscle maintenance to brain functions, the body requires a proper nutritional intake. According to Mozaffarian (2012), at least 30 vitamins, minerals, and dietary components are needed by the body that are not manufactured on its own in sufficient amounts. He adds that by acting in concert (synergism), these essential compounds perform thousands of roles in the body, ranging from healing wounds to boosting the immune system, converting food into energy, and repairing cell and tissue damage. Moreover, depending on the metabolic pathways and the structural components in which a nutrient is involved in the central nervous system (CNS), neuroanatomy, neurophysiology, and/or neurochemistry may be disrupted, each of which will result in altered neuronal function (Fuglestad, Ramel, & Georgieff, 2010). However, failing to get even those small quantities virtually guarantees a pathological state (Mozaffarian, 2012), which include behavioral consequences. Kaplan and Leung (2011), indicate that possibly psychiatric disorders are expressions of cumulative deficiencies of micronutrients required to manage oxidative stress.
Zimmermann (2001) identifies five mayor factors to the widespread vitamin and mineral deficiencies or insufficiencies: (a) loss of micronutrients due to food refining, processing, and storage, (b) soils depletion of minerals and trace elements due to modern intensive agricultural methods, (c) wrong dietary choices made by individuals, (d) polluted urban and industrial environments increase micronutrient requirements, and (e) medicinal drugs, as well as alcohol, tobacco, caffeine, all interfere with absorption and/or utilization of micronutrients. For example, a research conducted by O’Donnell et al (2008), found that only 3% of the kids meals offered by fast food companies met the National School Lunch Program guidelines, and the rest did not, and were also lower in energy density which contributed to the children’s unhealthy nutritional status. On a National Household Survey conducted by Bowman et al. (2008), to inquire about diet quality among children, the results showed that fast-food consumers ate more total fat and saturated fat, more total carbohydrate, more added sugars, more sugar-sweetened beverages, less milk, fewer fruits and non-starchy vegetables. On the other hand Brito Noronha, Almeida Cunha, Agra Araujo, Flaminio Abrunhosa, Nunes Rocha and Freitas Amara (2015) point out that undernutrition is a common problem in the elderly. This will also make them vulnerable to different conditions including mood and cognitive disorders.
.
The Brain, Lipids and Fatty Acids
Essentially all body functions including consciousness, thought, learning, memory, sleep, voluntary and involuntary behaviors, emotion, sensory perception and control of visceral function, are regulated or controlled by the nervous system (Tanner & Webster Ross, 2004). The brain is one of the organs with the highest level of lipids (Popa & Ladea, 2012), and has high metabolic requirements and is vulnerable to injury within minutes after interruption of it metabolic needs (Tanner & Webster Ross, 2004).
Omega-3 and 6 fatty acids are essential fats in the sense that the body cannot make them yet they should form part of our diet (Benton, 2007). In the brain, the levels of polyunsaturated fatty acids (PUFAs) are higher in the brain than in other organs (Benton, 2007). Brain lipids, composed of fatty acids, are structural constituents of membranes and it has been estimated that gray matter contains 50% (PUFAs) out of which about 33% belong to the Omega-3 family (Popa & Ladea, 2012). Therefore, being essential fatty acids, meaning that they cannot be synthesized in the body, they must be supplied through diet (Popa & Ladea, 2012). Kidd (2007), points out that the omega-3 fatty acids docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) are orthomolecular, conditionally essential nutrients that enhance quality of life, lower the risk of premature death, promote pre and postnatal brain development, have influence on behavior and mood, and generate neuroprotective metabolites. Early deficiencies in DHA and EPA may initiate the reduction of Serotonine levels in critical periods of neuronal development and affect the production and proper development of certain neurotransmitters, seriously hindering the regulation of the limbic system by the frontal cortex (Rodríguez, González & Miranda, 2008). In addition, there is biologically plausible evidence to suggest that omega-3 PUFAs might play a role as adjunctive therapy for depression, though much research is required to determine the most effective Omega-3 PUFA (EPA, DHA or a mixture of both) and the most effective dose (Popa, & Ladea, 2012). Furthermore Hamazaki et al. (1996), reported that the depletion of n-3 fatty acids from diets over two generations appear to affect the brain and retinal functions of animals. In their research Hamazaki et al. (1996), found that DHA intake prevented extraggression from increasing at times of mental stress.
Kidd (2007), indicates that in double blind, randomized, controlled trials, DHA and EPA combinations have shown benefits in conditions such as attention deficit/hyperactivity disorder (AD/HD), autism, dyspraxia, dyslexia, and aggression. On the other hand, food intolerance is one mechanism by which diet may influence anti-social behavior, and there is consistent evidence from well-controlled studies that some children with ADHD and related diagnoses respond adversely to food (Benton, 2007). In the case of affective disorders, meta-analyses confirm benefits of DHA and EPA in major depressive disorder (MDD) and bipolar disorder, with promising results in schizophrenia and initial benefit for borderline personality disorder (Kidd, 2007). On the other hand, accelerated cognitive decline and mild cognitive impairment (MCI) correlate with lowered tissue levels of DHA/EPA, and supplementation has improved cognitive function, while Huntington disease has responded to EPA (Kidd, 2007). In addition, a study conducted by Buydens-Branchey, Branchey, and Hibbeln (2008), suggested that by ensuring adequate n-3 PUFA intake via supplementation benefits substance abusers reduce their anger and anxiety levels. These findings are essential in understanding the biological substrates of violence. In fact, exaggerated aggressive responses can be observed in both high- and low-arousal states, with different biochemical and anatomical systems contributing to behavior in each context (Nelson & Trainor, 2007). Therefore, understanding the benefits of micronutrients in brain chemistry and general functioning is essential to produce a new approach to manage violence and its consequences.
B Vitamins
The B group of vitamins or B vitamins are coenzymes without which many body enzymes cannot function appropriately (Youngson, 2005; Youngson, 2006). According to Mozaffarian (2012), several epidemiological studies have exposed that blood concentrations of vitamins B6, B12, and folic acid are linked to people’s performance on tests of memory and abstract thinking. Moreover, folate and vitamin B12 deficiency can produce a megaloblastic anemia and demyelination in the spinal cord and brain, causing peripheral neuropathy, myelopathy, gait disturbance, incontinence, visual impairment, and neuropsychiatric syndromes (Scharre, 2007). However, administration of vitamin B12 may reverse or stop the progression of the neurological symptoms and dementia (Scharre, 2007). Folic acid supplements are valuable in preventing neural tube defects (Youngson, 2006). These vitamins have been pointed out by the literature as key elements for proper brain functioning and therefore adaptive social behavior.
.
Vitamin D
Vitamin D is a fat-soluble vitamin found in few foods and D3 is the form made naturally by the body in response to sunlight (Mozaffarian, 2012). Emerging evidence has linked vitamin D not only to its known effects on calcium and bone metabolism, but also to many chronic illnesses involving neurocognitive decline (Schlögl & Holick, 2014). Its supplementation may decrease depression symptoms by means of its beneficial effects on neurotransmitters, biomarkers of inflammation, metabolic profiles, and oxidative stress (Sepehrmanesh et al., 2016).
In a cross-sectional observational study of the records of 12,594 patients in a Mayo Clinic database, researchers identified a link between depression and low levels of Vitamin D (Mozaffarian, 2012). In a randomized clinical trial vitamin D supplementation of patients with Major Depressive Disorder (MDD) for 8 weeks had beneficial effects on the Beck Depression Inventory (BDI), indicators of glucose homeostasis, and oxidative stress (Sepehrmanesh et al., 2016).
Furthermore Vitamin D signaling is involved in brain development and function (Schlögl & Holick, 2014). On the other hand Ataie-Jafari, A., et al. (2015) indicate that according to their research some self-reported psychiatric distress such as anger, anxiety, poor quality sleep, sadness or depression, and worry are associated with hypovitaminosis D in adolescents. In a cross sectional study of serum 25-OHD levels in community dwelling individuals with established psychosis, Lally et al. (2016) found high level of vitamin D deficiency.
.
Sugar, Food Intolerance and Food Allergy
Sugars are part of nowadays culturally reinforced feeding habits. Most fast-foods contain high levels of sugar and salt disturbing the body’s internal chemistry. According to Benton (2007), there is evidence that a tendency to develop low blood glucose levels, higher than those that can be described as hypoglycaemic, is associated with irritability and violence. In his research Schoenthaler (1985) found that 1000 juvenile delinquents reduced their antisocial behavior by 44% when they were placed on a low sugar diet. This is a topic of special interest due to the brain’s requirement of glucose. In addition, allergic and intolerance to foods further hinder the body’s adequate functioning.
Even though micronutrients can function as immune modulators, foods and other nutrients may act as triggers of aberrant, innate immune reactivity, frequently manifesting as an allergy or sensitivity/intolerance (Pietschmann, 2015). According to Jiménez Ortega, Ortega Anta, Botija Arcos, & González Iglesias (2014) approximately 20% of the population will present an adverse food reaction of diverse types, including allergies and food intolerances throughout their life. This is a particular aspect of nutrition that should take into account and it is by itself a research topic given the many variables that affect food and produces intolerance and allergic reactions.
On the other hand, Dreborg (2015), indicates that the term “intolerance” should not be used within the area of allergy stating that intolerance requires a better definition and should be restricted to some non-immunological/non-allergic diseases and not mixed with allergy for example. In order to manage food intolerance and allergic reactions in individuals, restrictions to their diet are implemented. In fact, the primary treatment of these reactions is the full or partial restriction of the diet of foods and substances that produce those reactions (Jiménez Ortega, Ortega Anta, Botija Arcos, & González Iglesias, 2014). Therefore, establishing a correct diagnosis is essential in order to avoid unnecessary elimination diets, which in some cases could have negative consequences, leading to nutritional deficiencies and impaired growth and development (Jiménez Ortega, Ortega Anta, Botija Arcos, & González Iglesias, 2014).
.
Magnesium, Tryptophan and Serotonin
Tryptophan is an essential amino acid in higher organisms, but its abundance in proteins is relatively low (Bender, 1983) cited in Russo et al. (2009). Different suggestions have been made regarding the underlying cognitive and motivational processes that might be affected by tryptophan depletion, and therefore causing increased aggression (Krämer, Riba, Ritcher, & Münte, 2011). Moreover, low concentrations of a metabolite of serotonin found in cerebrospinal fluid (CSF), 5-hydroxyindolacetic acid (5-HIAA), are strongly associated with suicidal and violent behaviors (Hibbeln, et al. 2000). However, magnesium, a mineral essential in many functions of the body including the fact of it is used in the Krebs cycle and is a cofactor in the production of steroid hormones and neurotransmitters like serotonin (Rothfeld, 2003).
.
Discussion
As stated by Ramsey and Muskin (2013) an increasing amount of literature links dietary choices to brain health and the risk of psychiatric illness pointing to the fact that vitamin deficiencies can affect psychiatric patients in the following ways: a) deficiencies may play a causative role in mental illness and exacerbate symptoms, b) psychiatric symptoms can result in poor nutrition and c) vitamin insufficiency (defined as subclinical deficiency) may compromise patient recovery. However, this reality can produce significant consequences at the time that it is an essential part of a complex network of factors and variables we explain in the figure below.
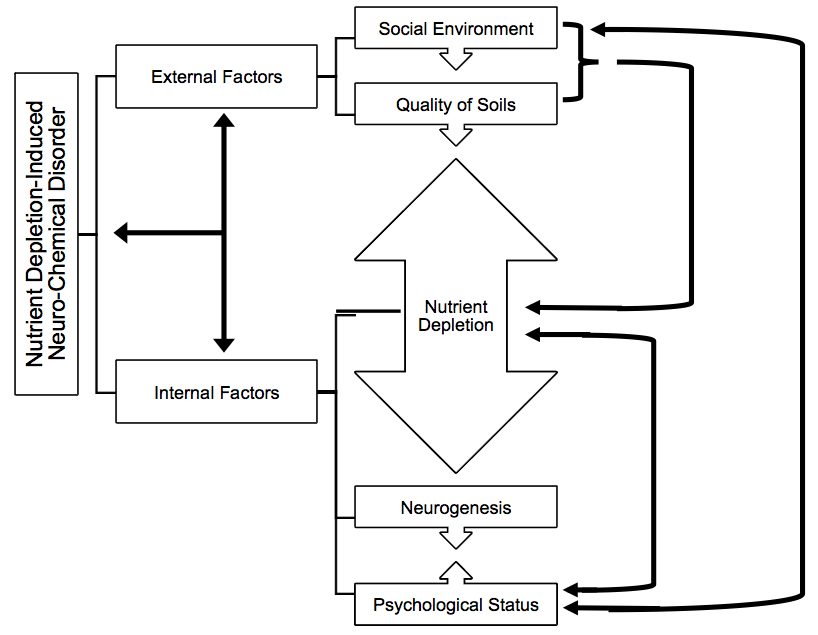
Figure 1. Relation of Internal and External Factors of Psychopathology and Aggressive Behavior in Relation to Nutrient Depletion-Induced Neuro-Chemical Disorder (Brain Hunger)
.
In face of the scientific literature found we believe there is an intricate yet logic relationship between internal and external factors related to psychopathology and aggressive behavior in that are the basis of what we have identified as Nutrient Depletion-Induced Neuro-Chemical Disorder (Brain Hunger). On one hand are the external factors of social environment and quality of soils and on the other the internal factors of nutrient depletion, neurogenesis and psychological status. Social environment encompasses many elements such as education, economy and geography which have an impact on the quality and management of soils. In turn there is a bilateral effect on nutrient depletion. At the same time nutrient depletion will have a direct effect on neurogenesis and psychological status. This interrelation will finally have an effect translated into mane behaviors including aggression and violence. In addition, this will make individuals more vulnerable to suffering from aggression too. Moreover, psychological conditions and status will affect the way people nurture themselves and it will represent another detrimental change in nutritional intake depleting the system of essential micronutrients for proper physical, neurocognitive and psychological functioning.
.
Conclusions
The body needs and stores fairly large amounts of major minerals including sodium, chloride, potassium, calcium, phosphorus and magnesium (Mozaffarian, 2012). The brain and nervous system require specific nutrients to function properly, and there is overwhelming evidence supporting the fact that nutrient deficiencies can lead to aggression and violent behavior (Onusic, 2013). Although the amounts of vitamins needed to maintain health are small and almost always present in normal and well balanced diets (Younsgon, 2006), nowadays patients are often overfed but undernourished (Ramsey & Muskin, 2013).
Having researched and scrutinized the scientific literature it is evident that there is a relationship between nutrition and human behavior (adaptive and maladaptive). Due to the human psychophysiological nature, emotional, social, biological and nutritional factors play an important role in overall behavior. Factors such as loss of micronutrients due processes like refining food, soil depletion of minerals, wrong dietary choices, pollution and interference of absorption due to medical drugs and other substances produce general nutritional deficiencies (Zimmermann, 2001). Furthermore, given the high rates of mental illness and violence, traditional protocols would benefit from a nutritional approach that would potentially aid in the treatment process, reduction of symptoms including aggression and promoting more stability. Therefore, nutritional depletion is a key factor in managing proper brain functioning, cognition, behavior and reduction of mental illness symptoms, and violence.
There is evidence for the interplay between malnutrition and neuro-disabling conditions (Gladstone et al. 2015). In addition, it is imperative to recognize that inflammation and oxidative stress are unavoidable components of even the most balanced system (Kaplan, Rucklidge, Romijn & McLeod, 2015). Also diet and nutrition has a complex relationship with mental health and there is evidence that specific micronutrients may have an effect on mood and depression, as well as the risk of developing and progress of dementia (Jennings, 2015), as well as other sub-clinical manifestations that include aggressive behavior. Therefore, nutritional intake takes a primary role in maintaining health and proper neurocognitive and behavioral functioning. Even though general nutritional status is difficult to evaluate (Rothfeld, 2003), it is essential to promote good nutritional intake as a form of promotion of health and prevention of “brain-hunger” which causes many neurocognitive and psycho-social consequences including psychopathology, aggression and violence. On the other hand, being the brain the center of control of physiological and neurocognitive functions, as well as psychological wellbeing, it requires a great deal of care to function properly. Therefore, Nutrient Depletion-Induced Neuro-Chemical Disorder (Brain Hunger) is a promising explanation and exploration topic which opens the door to a new transdisciplinary approach to the study of psychopathology and aggressive behavior, and the vulnerable position in which these individuals end up. Moreover, this is a encouraging path to potentially address the issue and improve neurocognitive, mental and social health and wellbeing.
.
References:
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders, Fifth Edition, Text Revision. Arlington, VA: Author.
Ataie-Jafari, A., et al. (2015). The association of vitamin D deficiency with psychiatric distress and violence behaviors in Iranian adolescents: the CASPIAN-III study. Journal of Diabetes & Metabolic Disorders. DOI 10.1186/s40200-015-0191-9
Benton, D. (2007). The impact of diet on anti-social, violent and criminal behavior. Neuroscience and Biobehavioural Reviews (In Press). doi:10.1016/j.neubiorev.2007.02.002
Bowman, S.A., Gortmaker, S.L., Ebbeling, C.B., Pereira, M.A., & Ludwig, D.S. (2008). Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics, 113(1), 112-118.
Brito Noronha, M., Almeida Cunha, N., Agra Araujo, D., Flaminio Abrunhosa, S., Nunes Rocha, A., & Freitas Amara, T. (2015). Undernutrition, serum vitamin B12, folic acid and depressive symptoms in older adults. Nutrición Hospitalaria, 32(1), 354-361.
Buss, D., & Shackelford, T. (1997). Human aggression in evolutionary psychological perspective. Clin Psyehoi Rev., 17(6), 605-619.
Buydens-Branchey, L., Branchey, M., & Hibbeln, J.R. (2008). Associations between increases in plasma n-3 polyunsaturated fatty acids following supplementation and decreases in anger and anxiety in substance abusers. Prog Neuropsychopharmacol Biol Psychiatry, 32(2), 568–575.
Davidson, K.M., & Kaplan, B.J. (2012). Nutrient intakes are correlated with overall psychiatric functioning in adults with mood disorders. The Canadian Journal of Psychiatry, 57(2), 85-92.
Dreborg, S. (2015). Debates in allergy medicine: food intolerance does not exist. World Allergy Organization Journal, 8, 37. doi 10.1186/s40413-015-0088-6
Fuglestad, A.J., Ramel, S.E., & Georgieff, M.K. (2010). Micronutrient needs of the developing brain. Priorities and Assessment. In. Packer, L., Sies, H., Eggersdorfer, M., & Cadenas, E. (Eds.). Micronutrients and brain health. (pp. 93-116). Florida, UCA: CRC Press-Taylor & Francis Group.
Gladstone, M., et al. (2015). Assessment of neurodisability and malnutrition in children in Africa. Seminars in Pediatric Neurology, 21, 50-57.
Grader, E., & Bateman, A. (2017). Introduction to brain anatomy and mechanisms of injury. In R. Winson, B.A. Wilson, & A. Bateman (Eds.), The brain injury rehabilitation workbook. (pp. 15-35). New York: Guilford Press.
Hamazaki, T., et al. (1996). The effect of docosahexaenoic acid on aggression in young adults. A placebo-controlled double-blind study. Journal of Clinical Investigation, 97(4), 1129-1134.
Hibbeln, J.R., Umhau, J.C., George, D.T., Shoaf, S.E., Linnoila, M., & Salem, N. (2000). Plasma total cholesterol concentrations do not predict cerebrospinal fluid neurotransmitter metabolites: implications for the biophysical role of highly unsaturated fatty acids. American Journal of Clinical Nutrition, 71, 331–338.
Hiday, V.A., Swartz, M.S., Swanson, J.W., Borum, R., & Wagner, H.R. (1999). Criminal victimization of persons with severe mental illness. Psychiatric Services, 50, 62-68.
Higging, E.S., & George, M.S. (2009). Brain stimulation therapies for clinicians. Washington DC: American Psychiatric Publishing, Inc.
Jennings, E. (2015). The importance of diet and nutrition in severe mental health problems. Journal of Community Nursing, 29(5), 68-73.
Jiménez Ortega, A.I., Ortega Anta, R.M., Botija Arcos, G., & González Iglesias, M.J. (2014). Intolerancias alimentarias; retos en la mejora. Nutrición Hospitalaria,30(2), 91-97.
Kaplan, B.J., Fisher, J.E., Crawford, S.G., Field, C.J., Kolb, B. (2004). Improved mood and behavior during treatment with a mineral-vitamin supplement: An open-label case series of children. Journal of Child and Adolescent Psychopharmacology, 14(1), 115-122.
Kaplan, B. J., & Leung, B. (2011). Micronutrient treatment of mental disorders. Integrative Medicine: A Clinician’s Journal, 10(3), 32-39.
Kaplan, B.J., Rucklidge, J.J., Romijn, A., & McLeod, K. (2015). The emerging field of nutritional mental health: inflammation, the microbiome, oxidative stress, and mitochondrial function. Association for Psychological Science, 1-17. doi: 10.1177/2167702614555413
Keunen, K., van Elburg, R.M., van Bel, F. & Benders, M.J.N.L. (2015). Impact of nutrition on brain development and its neuroprotective implications following preterm birth. Pediatric Research, 77, 148–155. doi:10.1038/pr.2014.171
Kidd, P.M. (2007). Omega-3 DHA and EPA for cognition, behavior, and mood: Clinical findings and structural-functional synergies with cell membrane phospholipids. Alternative Medicine Review 12(3), 207-221.
Krämer, U.M., Riba, J., Ritcher, S., & Münte, T.F. (2011). An fMRI study on the role of serotonin in reactive aggression. PLoS ONE, 6(11), 1-8.
Krug, E., et al., (2002). World Report on Violence and Health. Geneva: World Health Organization.
Lally, J., Gardner-Sood, P., Firdosi, M., Iyegbe, C., Stubbs, B., Greenwood, K., & … Gaughran, F. (2016). Clinical correlates of vitamin D deficiency in established psychosis. BMC Psychiatry, 161-9. doi:10.1186/s12888-016-0780-2
Magnativa, J.J., Powers, A.D., Barber, J.P., & Oltsmanns, T.F. (2013). Personality disorders. In. L.G. Castonguay, & T.F. Oltmanns (Eds.), Psychopathology. From science to clinical practice. (pp. 275-318). New York: Guilford Press.
McCabe, P.C., & Shaw, .S.R. (2010). Developments in neuropsychiatric treatment. In. McCabe, P.C., & Shaw, S.R. (Eds.), Psychiatric disorders. Current topics and interventions for education. (pp. 2-7). California, USA: National Association of School Psychologists & CORWIN.
Mendes et al. (2009). Estudo de revisâo dos fatores biológicos, sociais e ambientáis associados com o comportamento agressivo. (Portuguese). Study review of biological, social and environmental factors associated with aggressive behavior. Revista Brasileira de Psiquiatria 31(2), 77-85.
Mercadillo, R.E., & Arias, N.A. (2011). Violence and compassion: a bioethical insight into their cognitive bases and social manifestations. International Social Science Journal 221-232.
Mozaffarian, D. (2012). The truth about vitamins and minerals. Choosing the nutrients you need to stay healthy. Boston, USA: Harvard Health Publications.
Nelson, R.J., & Trainor, B.C. (2007). Neural mechanisms of aggression. Nature 8, 536-546.
O’Donnell, S.I., Hoerr, S.L., Mendoza, J.A., & Tsuei Goh, E. (2008). Nutrient quality of fast food kids meals. The American Journal of Clinical Nutrition, 88, 1388-1395.
Okami, P., & Shackelford, T. (2001). Human sex differences in sexual psychology and behavior. Ann Rev Sex Res, (12), 186-241.
Oltmanns, T.F., & Castonguay, L.G. (2013). General issues in understanding and treating psychopathology. In L.G. Castonguay, & T.F. Oltmanns (Eds.), Psychopathology. From science to clinical practice. (pp. 1-16). New York: Guilford Press.
Onusic, S. (2013). Violent behavior: A solution in plain sight. Recovered August 5, 2016 from The Weston A. Price Foundation http://www.westonaprice.org/uncategorized/violent-behavior-a-solution-in-plain-sight/
Pietschmann, N. (2015). Food intolerance: Immune activation through diet-associated stimuli in chronic disease. Altern Ther Health Med, 21(4), 42-52.
Pliszka, S.R. (2016). Neuroscience for the mental health clinician. (2nd ed). New York: The Guilford Press.
Popa, T.A., & Ladea, M. (2012). Nutrition and depression at the forefront of progress. Journal of Medicine and Life, 5(4), 414‐419.
Ramsey, D., & Muskin, P.R. (2013). Vitamin deficiencies and mental health: How are they linked? Identifying and correcting deficiencies can improve brain metabolism and psychopathology. Current Psychiatry, 12(1), 37-44.
Rodríguez, J.R., González, M.J., & Miranda, J. (2008). Deficiencias nutricionales y comportamientos inadaptados: un posible nuevo paradigma para la prevención de conductas agresivas. Psicología y Salud, 18(2), 199-206.
Rothfeld, G.S. (2003). Nutrition. In. Leskowitz, E., & Micozzi, M.S. (Eds,), Complementary and alternative medicine in rehabilitation. Medical guides to complementary and alternative medicine series. (pp. 84-96). St. Louism, Missouri, USA: Churchill Livingstone
Rucklidge, J.J., Harrison, R., & Johnstone, J. (2011). Can micronutrients improve neurocognitive functioning in adults with ADHD and severe mood dysregulation? A Pilot Study. The Journal of Alternative and Complementary Medicine, 17(12), 1125-1131.
Russo, S., Kema, I.P., Bosker, F., Haavik, J, & Korfi, J. (2009). Tryptophan as an evolutionarily conserved signal to brain serotonin: Molecular evidence and psychiatric implications. The World Journal of Biological Psychiatry, 10, 258-268.
Scharre, D.W. (2007). Infectious, Inflammatory, and Demyelinating Disorders. In. Miller, B.L., & Cummings, J.L. (Eds.). The human frontal lobes. Functions and disorders. (2nd ed.). (pp. 518-539). New York: The Guilford Press.
Sepehrmanesh, Z., Kolahdooz, F., Abedi, F., Mazroii, N., Assarian, A., Asemi, Z., & Esmaillzadeh, A. (2016). Vitamin D supplementation affects the Beck Depression Inventory, insulin resistance, and biomarkers of oxidative stress in patients with major depressive disorder: a randomized, controlled clinical trial. Journal of Nutrition, 146(2), 243-248. doi:10.3945/jn.115.218883
Siever, L.J. (2008). Neurobiology of aggression and violence. American Journal of Psychiatry 165, 429–442.
Silver, J.M., & Yudofsky, S.C. (1997). Violence and the brain. In T.E. Feinberg, & M.J. Farah (Eds.). Behavioral neurology and neuropsychology. (pp. 711-717). USA: McGraw-Hill.
Schoenthaler, S.J. (1985). Diet and delinquency: Empirical testing of seven theories. International Journal of Biosocial Research, 7(2), 108-131.
Schlögl, M. & Holick, M (2014). Vitamin D and neurocognitive function. Clinical Interventions in Aging, 9, 559–568.
Tanner, C.M., & Webster Ross, G. (2004). Neuroepidemiology: Fundamental considerations. In. Nelson. L.M., Tanner, C.M., Van Den Eeden, S.K., & McGuire, V.M. (Eds.), Neuroepidemiology. From principles to practice. (pp. 1-22). New York: Oxford University Press.
Umhau, J.C., Trandem, K., Shah, M., & George, D.T. (2012). The physician’s unique role in preventing violence: a neglected opportunity? BMC Medicine 10(146), 1-8.
Wakefield, J. C. (2010). Taking disorder seriously: A critique of psychiatric criteria for mental disorders from the harmful-dysfunction perspective. In T. Millon, R. F. Krueger, & E. Simonsen (Eds.), Contemporary directions in psychopathology: Scientific foundations of the DSM-V and ICD-11 (pp. 275-302). New York: Guilford Press.
Waters, H., Hyder, A., Rajkotia, Y., Basu, S., Rehwinkel, J.A., & Butchart, A. (2004). The economic dimensions of interpersonal violence. Department of Injuries and Violence Prevention. Geneva: World Health Organization.
Watson, N.V., & Breedlove, S.M. (2012). The mind’s machine. Foundations of brain and behavior. Sunderland, Massachussets, USA: Sinauer Associates, Inc. Publishers.
Youngson, R.M. (2005). Collins dictionary of medicine. Medicine defined and explained. (4th ed.). London: Harper Collins Publishers.
Youngson, R.M. (2006). Collins dictionary of human biology. Human biology defined and explained. London: Harper Collins Publishers.
Zaalberg, A., Nijman, H., Bulten, E., Stroosma, L., & van der Staak, C. (2009). Effects of nutritional supplements on aggression, rule-breaking, and psychopathology among young adult prisoners. Aggressive Behavior, 35, 1–10.
Zimmermann, M. (2001). Burgerstein’s handbook of nutrition. Micronutrients in the prevention and therapy of disease. New York: Thieme.


