.
Shortcomings of evidence-based medicine, revealed in COVID-19 mismanagement
One of the major concerns with evidence-based medicine (EBM) is the gradually increasing bias in what constitutes as evidence. Another is the lack of mechanistic or logical reasoning. The third is what I consider as the dominance of a “Nobel prize mentality” in today’s clinical medicine, i.e., using narrowly focused basic science research principles and tools to address complex and holistic problems. The medical mismanagement of COVID-19 illustrates these concerns, and is clearly creating additional problems beyond the direct impact of the virus itself.
The current evidence-based medicine movement, started in the 1990s, has gradually become the central dogma of today’s medical practice. Throughout the history of medicine, there has always been a focus on combining empirical (or experience-based) medicine with evidence generated through academic research. EBM had become increasingly reliant on academia when establishing the standard of care, despite the fact that ~50% of what a clinician does is still based on empirical medicine. As a result, we must question what is considered as evidence.
What is evidence-based medicine?
Evidence-based medicine is interpreted as the integration of best research evidence with clinical expertise and patient values. EBM aims for the ideal that healthcare professionals should make conscientious, explicit, and judicious use of current best evidence in their everyday practice” (Hines, n.d.).
Randomized controlled clinical trials (RCTs) are only part of the evidence in EBM
From a practical standpoint, there are several different levels of evidence in EBM – from RCTs to case studies, to emperial clinical experience (Tenny & Varacallo, 2020). It’s clear that although RCTs have the highest weight as evidence, they are not the only evidence to be utilized in EBM. However, a majority of the scientists and medical doctors whom I have communicated with focus on RCT data as the only evidence. They seem to exclude other levels of evidence, and think that if there is no RCT data, then it’s not EBM. To be clear, I didn’t know exactly what EBM was until I looked it up in the literature. I venture to say that this is quite common among scientists and clinicians.
RCT results and treatment guidelines contain limitations and financial conflicts which may result in bias. We as clinicians must still reason through the best choices for an individual patient even in the absence of full and secure knowledge. (Sniderman AD et al., 2013) SARS-Cov-2 is a novel virus, but it doesn’t mean we know nothing in the treatment and prevention of COVID-19. Even without thorough research, there is plenty we already know about viral infections that we can apply in both their prevention and treatment.
The increasing trend of biased evidence in support of for-profit, patentable drugs in EBM
Publicly funded RCTs have been declining, while for-profit industry funded RCTs are on the rise, a trend with a deep and biased influence on our healthcare policy, with potentially grave consequences.
Well-designed RCT results are considered the strongest evidence in EBM. Randomized clinical trials are very costly and their development is becoming increasingly limited to organizations with strong financial backing. A 2015 Johns Hopkins University study found the number of clinical trials funded by for-profit industry increased 43% while those funded by the NIH decreased by 24%, between the years 2006 and 2014. (Ehrhardt, Appel & Meinert, 2015) While the goals of NIH-funded RCTs are not to make a profit on the market, the industry funded RCTs are clearly for the purpose of profit.
There is no doubt that lifestyle and nutrition play fundamentally important roles in the maintenance of health, disease prevention, and treatment. However, lifestyle and nutritional research results are usually not patentable. There is no financial incentive for industry to conduct RCTs. This creates a bias towards their under representation in the evidence database that EBM relies on.
With a growing dominance of for-profit industry sponsored RCTs making up the “best evidence” in EBM, no wonder, medical practice today is biased and heavily influenced by pharmaceutical interests.
Some other facts:
- For-profit industry does not fund the trials which are most important for public health due to lack of financial incentive (Cohn, 2015). This includes the lifestyle and nutritional medicine, as discussed above.
- The Johns Hopkins University’s Comprehensive Cancer Center found conflicts of interest in more than one-third of 1,500 cancer studies published in prominent medical journals in 2006 (Cohn, 2015).
- As many as 70% of approved drugs are not new drugs, resulting in billions of dollars being spent on unnecessary clinical trials (Quigley, 2017).
Today’s clinical medicine has been dominated by basic science (Nobel prize mentality)
The Nobel prize is the crown jewel that attracts top medical and biological scientists. Those who reach the top of various medical specialties have spent most of their careers in basic research. There is a dichotomy between those who lead in medicine and those who actually practice medicine. Those influential medical experts, who develop disease management guidelines, and influence healthcare policies, are mostly attracted and dominated by the “Nobel prize mentality”. This disturbing trend is partly illustrated in the gradual decrease of Nobel prizes awarded to clinicians over the past 100 years (Fig. 1).
The proportion of clinicians to win Nobel prize in physiology and medicine has declined from 65%-90% around 100 years ago, to a merely 20% in the 21st century (Ashrafian et al., 2011). While basic research is important, only about 1% of the highly promising basic research is translated into clinical medical practice (Contopoulos-Ioannidis et al., 2003). Today’s Nobel prizes may not be what Mr. Alfred Nobel intended in his will. Over 100 years ago the Nobel committee interpreted Mr. Nobel’s will as: “the domain of physiology or medicine” which was understood to encompass the theoretical as well as the practical medical sciences (Ashrafian et al., 2011; Alfred Nobel’s Health, n.d.).
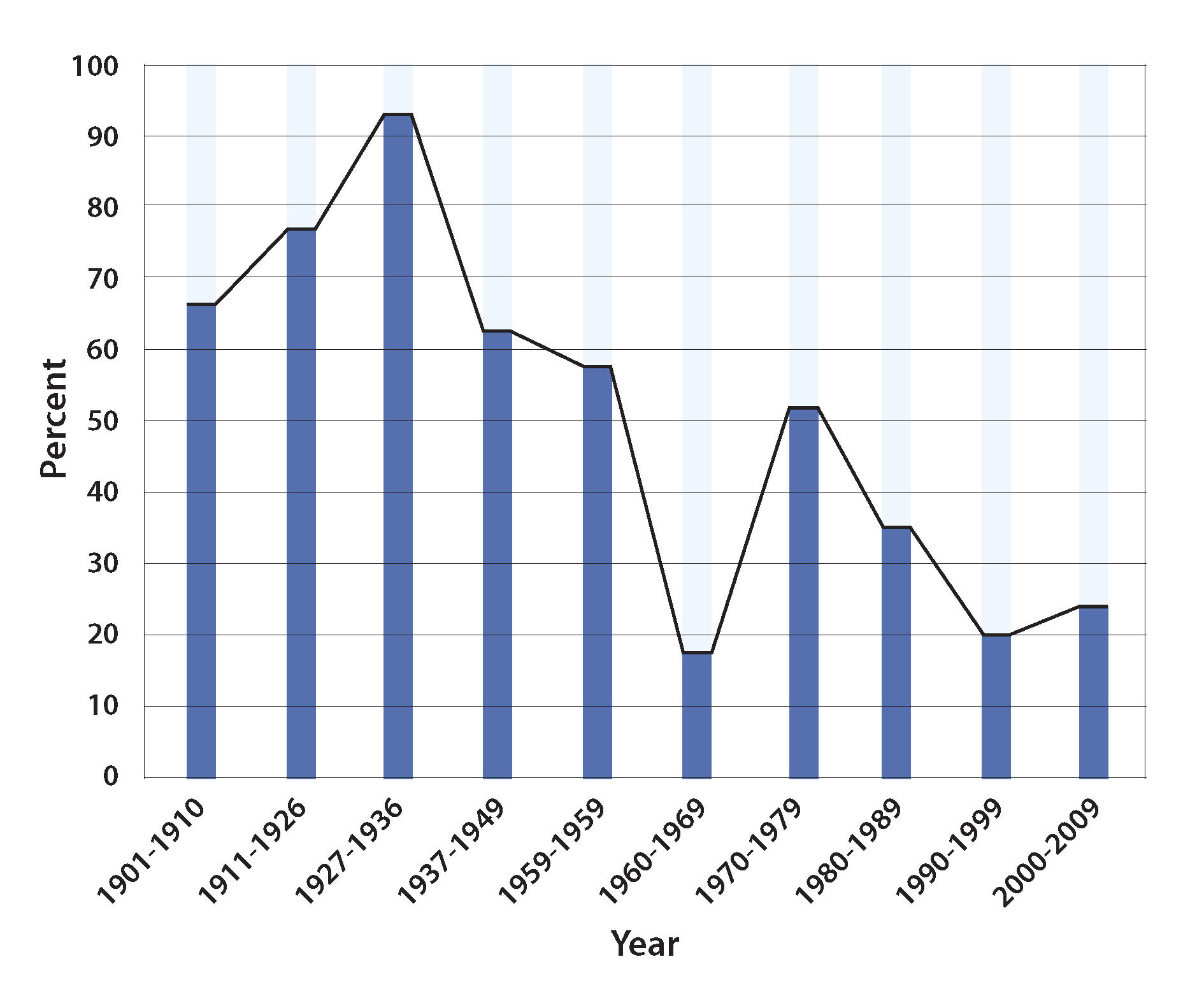
Fig. 1. Nobel Prizes in medicine: are clinicians out of fashion?
Source: Ashrafian H, Patel VM, Skapinakis P & Athanasiou T. (2011) J R Soc Med. 104, 387–389.
The approaches to clinical medicine and to basic medical research are and should be different. Basic research is to dissect complex problems into smaller and unit level questions, often looking at a particular molecule or a mechanism, irrespective of the whole system. Whereas clinical medicine should integrate the knowledge acquired from various sources into a holistic treatment plan for the individual patient. Clinical medicine should understand the patient as a whole, trying to identify not only the clinical manifestations, but also the root causes as well as the processes connecting the root causes and the clinical presentations (Fig. 2). Only when we address the root causes, the disease processes, and the clinical manifestations, will it become possible to cure the patient.
All disease has a root cause, which via certain pathological mechanisms or processes leads to clinical signs and symptoms (Fig. 2). Research on the root causes and management of disease is most viable when it focuses on specific patentable agents (drugs) to manipulate pathological mechanisms. As a result, the medical literature is full of research papers studying the biological processes, which may lead to new drug discoveries and ultimately financial benefits. We know clearly, intervention at the mechanism level, not at the root cause level, is only part of a disease management plan and can not provide a complete solution. Medical education and the current standard of care is based on one or a few drugs, resulting in an incomplete treatment plan, which does not address the root causes of disease. Although the market is full of redundant drugs for common chronic diseases such as diabetes mellitus and hypertension, none of these chronic diseases are curable with pharmaceutical intervention. More and more clinical research shows that chronic diseases such as diabetes and hypertension are reversible with lifestyle changes including dietary changes (Athinarayanan et al., 2020; Dong et al., 2019; van Namen et al., 2019; Kord-Varkaneh et al., 2020). We have helped numerous diabetic and hypertensive patients improve disease outcomes, often without the use of drugs, using an integrative approach. Unfortunately, this approach is not well-supported by the mainstream medical literature and key opinion leaders.
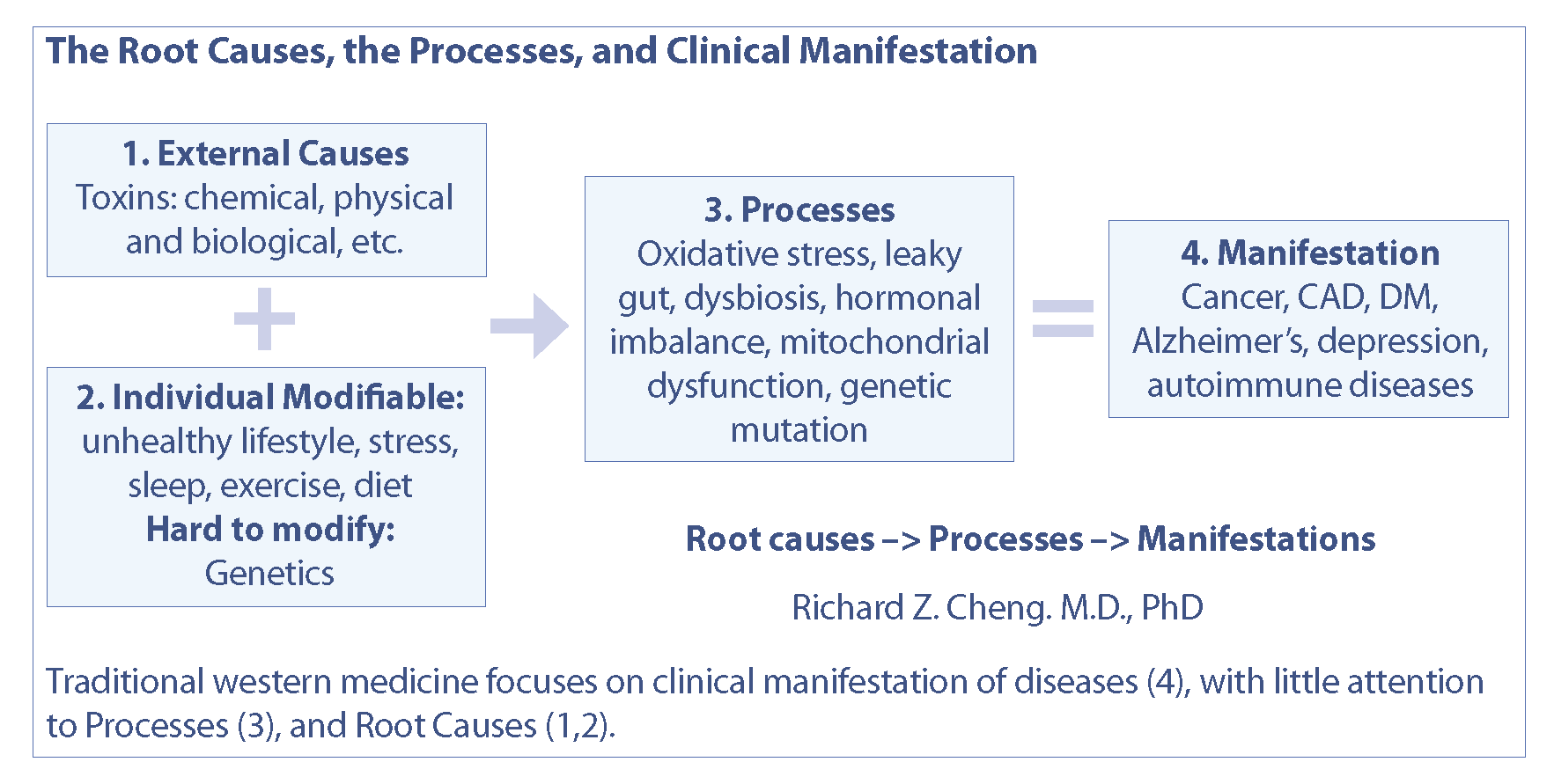
Fig. 2. The root causes, processes and clinical manifestations of diseases.
Worldwide reactions to the management of COVID-19 reveals severe problems
Management of this worldwide pandemic has been severely politicized. This is evident both internationally and domestically. Politics have hijacked the potential for a unified public health approach, causing unnecessary chaos and resulting in mismanagement with severe consequences.
Medical advisors to governments worldwide, including World Health Organization, have been providing incomplete medical advice. This situation has the potential to mislead to government representatives and local health authorities. Public health officials carry the major responsibility of assessing and analyzing the situation and synthesizing a comprehensive strategy to mitigate damage cause by the pandemic.
What have the public health officials, top medical agencies and advisors to the governments done to fight the COVID-19 pandemic? What we have seen and heard is a lot of confusion, disagreement, and the universal expectation of developing a vaccine. None of the top experts or medical agencies are talking about nutritional intervention and it’s importance in the prevention and treatment of COVID-19. Human health, including immune system functioning, is dependant on nutrition. This is well established. In the absence of specific “anti-COVID” drugs, our inate and acquired immunity is all we have to hold the virus at bay. Even with specific drugs, our immunity still plays a major role in fighting disease. Why don’t the top experts openly recommend nutritional intervention? Dr. Anthony Fauci, the top medical advisor to the Trump Administration, is reportedly taking vitamins C and D, but has not clearly recommended it for the public (“How to Avoid,” 2016). Numerous healthcare practitioners and advocates have been censored for recommending the evidence-based use of micronutrients. I am one of the victims of censorship. I have never seen medicine to be so politicized in my 40 plus years in practice.
I came across Dr. Linus Pauling’s work on vitamin C about twenty years ago. In recent years, I have spent more time researching vitamin C and it’s biological effects on nearly every aspect of health, including, but not limited to it’s antimicrobial properties, and antioxidant capacity (Levy, 2017).
Disturbance of redox homeostasis, resulting in increased oxidative stress, is the key underlying pathology of viral infections
A common feature of many viral infections, including the upper and lower respiratory infections caused by respiratory viruses is the disturbance of redox homeostasis, or increased oxidative stress. Redox homeostasis describes the balance between the production of reactive oxygen species (ROS), and reactive nitrogen species (RNS). Redox biology plays a critical role in various cellular processes, including proliferation, differentiation, signaling, and metabolism. Redox homeostasis and the disturbance thereof plays an important role in pathology and may lead to oxidative stress, chronic activation of immune responses, and inflammation (Mittal, et al., 2014; van der Vliet & Janssen-Heininger, 2014). Chronic elevation of ROS may lead to oxidative damage to DNA, proteins, and lipids, resulting in dysfunction of organelles and apoptosis. (Circu & Aw, 2010).
The group of viruses that may cause respiratory infections includes influenza, human respiratory syncytial virus, human rhino-, human metapneumo-, parainfluenza-, adeno- and corona-viruses (SARS-Cov). The latter includes the virus responsible for COVID-19, SARS-Cov-2, a novel member of the coronaviruses.
The medical literature contains a large body of evidence that demonstrates the correlation between the significant increase in ROS and most, if not all, viral respiratory infections (Khomich, 2018). Moreover, elevated ROS is not the only a feature of respiratory infections, but is also present in other viral infections such as hepatitis B and C, and many others. COVID-19 is no exception. Early research shows SARS-Cov-2 infection is associated with significantly increased oxidative stress, often described as “cytokine storm”.
The powerful antioxidant effects of vitamin C can explain the clinical improvement observed in pneumonia, sepsis and respiratory distress (Cheng, 2020a; Schönrich et al., 2020; Delgado-Roche & Mesta, 2020; Zarbafian et al., 2020).
Key pathologies of COVID-19 and mechanisms of vitamin C in the treatment of viral infections
- Vitamin C can prevent and improve the common cold and pneumonia
.
A meta-analysis of 148 animal studies show that vitamin C can alleviate or prevent bacterial, viral and protozoan infections. Vitamin C cuts the risks of colds by 50% in physically active adults. Two randomized and controlled (RCT) studies show a dose-dependent response in the therapeutic effects of vitamin C in common colds. A recent Korean study showed that vitamin C at doses as high as 6,000 mg daily reduced the odds of developing common cold. (Kim et al., 2017) Three RCTs demonstrate that vitamin C can prevent pneumonia and 2 RCTs show vitamin C can improve pneumonia treatment (Hemilä, 2017).
. - High dose intravenous vitamin C (HDIVC) shortens mechanical ventilation
.
HDIVC improves severe pneumonia patients. A recent meta-analysis pooled the data from 9 qualified clinical trials and found strong evidence that high dose IV vitamin C shortens patient time on mechanical ventilation by 14-25% with only relatively small vitamin C doses of 1,000 mg-6,000 mg (Hemilä & Chalker, 2020).
. - HDIVC reduces mortality in patients with acute respiratory distress syndrome (ARDS) and in COVID-19 patients
.
In a clinical trial of 32 ARDS patients, HDIVC (1,000 mg + N-acetyl cysteine + selenium + vitamin E, every 6 hours IV) showed a 47% reduction in mortality rate compared to the 71% mortality rate in the control group (Sawyer et al., 1989). Another recent study of 96 septic patients with HDIVC (6,000 mg of vitamin C + hydrocortisone + thiamine, every 6 hours IV) cut the mortality rate by ~32% (Marik et al. 2017). HDIVC for the treatment of COVID-19 was first reported in China. In a clinical study of 54 severe to critically ill COVID-19 patients shows HDIVC (24,000 mg/24 hours IV) reduced 28-day mortality and significant improvement of oxygenation and inflammatory status. In a separate clinical series study of 12 severe and critical COVID-19 patients, HDIVC showed significant clinical oxygenation improvement with reduction in inflammatory markers and organ failure (SOFA) score (Cheng, 2020d)
. - Vitamin C deficiency is more common than we realized, both in sick patients and in the general population
.
Vitamin C deficiency is common among patients with acute and chronic diseases. 40% of ICU patients with septic shock have blood levels of vitamin C near zero, diagnostic of scurvy (<11 umol/L), with the remainder of ICU patients have hypovitaminosis C (<23 umol/L). Low plasma vitamin C levels are associated with more severe organ failure and increased mortality (de Grooth et al., 2014; Vincent et al., 1996). ~50% of non-septic ICU patients also show hypovitaminosis C. Hypovitaminosis C is relatively common in Western populations and vitamin C deficiency (<11 umol/L) is the 4th leading nutrient deficiency in the US (Carr et al., 2017). The 2007-2010 U.S. National Health and Nutrition Examination Survey of approximately 16,000 children and adults found that almost 40% had low levels of vitamin C, while 88% of the U.S. population did not meet the daily requirement for vitamin E which is noted to enhance the effects of vitamin C (“Unusual” IV High-Dose, 2020).
. - COVID-19 patients have undetectable or very low blood levels of vitamin C
.
Vitamin C was not detectable in 17 out of 18 COVID-19 patients with ARDS, a Spanish study reports, with the remaining patient showing very low blood vitamin C level (Chiscano-Camón et al., 2020).
. - Vitamin C is safe and is without significant side effects, even at very high doses
.
An NIH expert panel consensus document (updated in February 2020) clearly states that HDIVC is safe even at very high doses. Early clinical studies show HDIVC is highly promising in COVID-19 treatment (Cheng, 2020a; Cheng, 2020b; High-Dose Vitamin C, 2013; Cheng, 2020e; Cheng et al., 2020; de Grooth et al., 2014). Based on these and their clinical experience of HDIVC, the governments of Shanghai and Guangdong officially included HDIVC in their Covid-19 treatment protocols. (Saul, 2020; Cheng, 2020c) The science and rationale for HDIVC in treatment of COVID-19 were reviewed and presented in my NIH guest speech (Cheng, 2020f). These early Chinese experiences in HDIVC on Covid-19 caused worldwide interest which was in part kicked off by the ITM Ltd. and The First Dragon Foundation™ Ltd., organizations who issued the global release (ITM: The Treatment, 2020) that also included introduction to the new US Federal “Right to Try Act”. According to the peer-reviewed Orthomolecular Medicine News Service, vitamin IVs can be arranged in virtually any hospital, anywhere in the world, and the new federal “Right to Try Act” gives patients the power to demand IV vitamin C treatment (Saul & Yanagisawa, 2020).
Are vaccines the answer to the COVID-19 pandemic?
It is clear that epidemics and pandemics are on the rise. COVID-19 is just a wake-up call. Due to the nature of vaccine research and development, there is always a significant delay between the outbreak of an epidemic and the wide availability of effective vaccines. Eleven months into the COVID-19 pandemic and there are no widely available SARS-Cov-2 vaccines. This despite the fact that all governments worldwide are investing in vaccines. A vaccine-only COVID-19 strategy undermines the viability of an integrative medical approach.
For protected population immunity it is imperative to incorporate recommendations for a healthy lifestyle and optimal nutrition, especially the supplementation of vitamins C, D, magnesium, and zinc (Cheng, 2020e; Levy, 2020).
Conclusion
The current medical approach focuses on symptomatology and often fails to address the root causes and common biological interventions for disease. This view of disease is conveniently compatible with a limited understanding of evidence-based medicine, and the identification of more diseases which perpatuate research grants and drug development. This is also conveniently compatible with pharmaceutical interests wherein more drugs can be utilized in the marketplace.
Evidence-based medicine is the main school of thought that guides the clinical medicine of today. A review of the definition of evidence-based medicine illustrates that logic or common sense have a limited place in EBM (Hines K, n.d; Tenny & Varacallo, 2020).
While COVID-19 is a novel form of the SARS-Cov virus, we can not discount what we have learned from the previous research on viruses and disease. Many viral infections, particularly the family of coronaviruses including the viral agents that caused the 2003 SARS pandemic, and the MERS pandemic in 2013, share much in common. Elevated oxidative stress, or the cytokine storm, is hallmark of disease progression (Cheng, 2020a; Cheng 2020e). Most, if not all, of the pathologies seen in COVID-19 can be traced to the oxidative damage induced by SARS-Cov-2. This is the rationale for using antioxidant treatments, especially high dose intravenous vitamin C.
Vitamin C, taken both orally or intravenously, is very safe and is effective in the prevention and treatment of both mild and severe viral infections. Other micronutrients that play a role in immune function have similar safety profiles and sufficient evidence to support their use in the prevention and treatment of COVID-19.
Many lives would be saved should the governments start to incorporate nutritional intervention into the prevention and treatment of COVID-19. This has been clearly established through the work we have done in Shanghai and Guangdong, China. Entire cities don’t have to be locked down. The economy can be revived more rapidly.
References


