Introduction
The Canadian Cancer Statistics Report presented 137 different types of blood cancers and blood disorders affecting the blood cells, bone marrow, lymph nodes and lymphatic system [1]. Currently estimated at 138,100 Canadians and increasing are living with or in remission from blood cancers [1]. There is a rise in evidence for non-malignant blood disorders [1]. Blood-related malignancies have the biggest increases in survival due to improvements in treatment [1]. This highlights the importance of identifying and classifying various blood disorders, especially to classify it as malignant or non-malignant.
Pancytopenia is a triad of cytopenias characterized by simultaneous reduction of erythrocytes, leukocytes and platelets2. Various causes of this phenomenon include, but are not limited to bone marrow failure, autoimmune-related destruction of cells, or sequestration in reticuloendothelial system [3,4]. Bone marrow failure is most commonly due to malignancy resulting from aplastic anemia (reduced hematopoietic stem cell production), myelodysplastic syndromes, acute leukemia and fibrosis of bone marrow [3,4]. Other than bone marrow disorders, other possible etiologies of pancytopenia include splenomegaly, sepsis, alcoholic diseases, systemic lupus erythematosus, nutritional deficiency (folate, B12), endocrine diseases and infectious causes (tuberculosis, leishmaniasis, brucellosis, hepatitis viruses, human immunodeficiency virus) [4,5]. Pancytopenia due to vitamin B12 deficiency can be completely reversed if treated early [5].
The clinical outcome of treatments provided highly depends on severity of symptoms, age of the patient, and etiology [4]. There is contradicting evidence on use of bone marrow biopsy in identifying etiology of pancytopenia [3]. Some common etiologies can be determined from laboratory analysis and radiological imaging, minimizing need for bone marrow biopsy [5]. Untreated pancytopenia could progress to life-threatening infection or uncontrolled bleeding in late stages of the disease [2]. Management and prognosis of blood disorders is complex and depends on pathophysiology and patient health status [4]. The vast possible causes of pancytopenia highlight the importance of quickly and efficiently identifying etiology in order to provide essential treatment and appropriate management [4].
This current case report is classified as unusual due to the presence of pancytopenia alongside multiple other blood abnormalities, such as poikilocytosis, risk of anemia (low B12 and Iron), elevated gamma globulin, elevated erythrocyte sedimentation rate (ESR), elevated immunoglobulins and lowered alanine aminotransferase. The vast and vague symptom presentation that improves with certain naturopathic treatments suggests possible concurrent nutritional deficiencies, which will be discussed in this case report. One case study on splenomegaly and pancytopenia was found that is significantly similar to this case; however it was an end-stage study where the patient was diagnosed with a carcinoma of the tail of the pancreas [6].
Case Presentation
Demographic Information
This case report describes a 48-year-old Asian female born and raised in Africa. She relocated to Canada in the 1980s. Her managerial position in her field of work involved frequent travel across Canada since early 2000s up until 2019, and now she is mainly stationed in one location. She is a successful businesswoman employed in a manager position at a high-stress workplace environment. The patient presented at the Robert Schad Naturopathic Clinic (RSNC) with a chief complaint of an unknown autoimmune condition causing abnormal values on blood work that are worsening.
Biopsychosocial Determinants of Health
The patient lives alone at home, however she does maintain contact with neighbours and friends frequently. She describes work as stressful in waves, and she reports she does not handle stress well. In response, she describes herself as an anxious person. The anxiety was reported to be fueled by recent deaths of loved ones (due to pancreatic cancer and renal failure) and her personal blood reports showing abnormal values. The patient supported both parents through their terminal illnesses and end of life decisions throughout 2015-2019. She has yet to be given a clear formal diagnosis of the disease by her hematologist. The vague presentation of the disease is impacting her psychological health in terms of her motivation, anxiety levels and thoughts about her future life situation. Her perspective on her illness is determined by her anxiety levels and her trust in reaching out to healthcare professionals for support versus online resources. Currently, she reported being relieved that her current hematologist opinion supported the previous two hematologists’ expert opinions. A bone marrow biopsy was deemed not required at the moment, and the patient is set on a 6-month follow up schedule to keep track of abnormal values. She presented signs of gratitude and appreciation that she has so many healthcare providers working with her and supporting her health. She is focusing on valuing her health as a priority, and is making more conscious decisions about any work or personal life choices that impact her health.
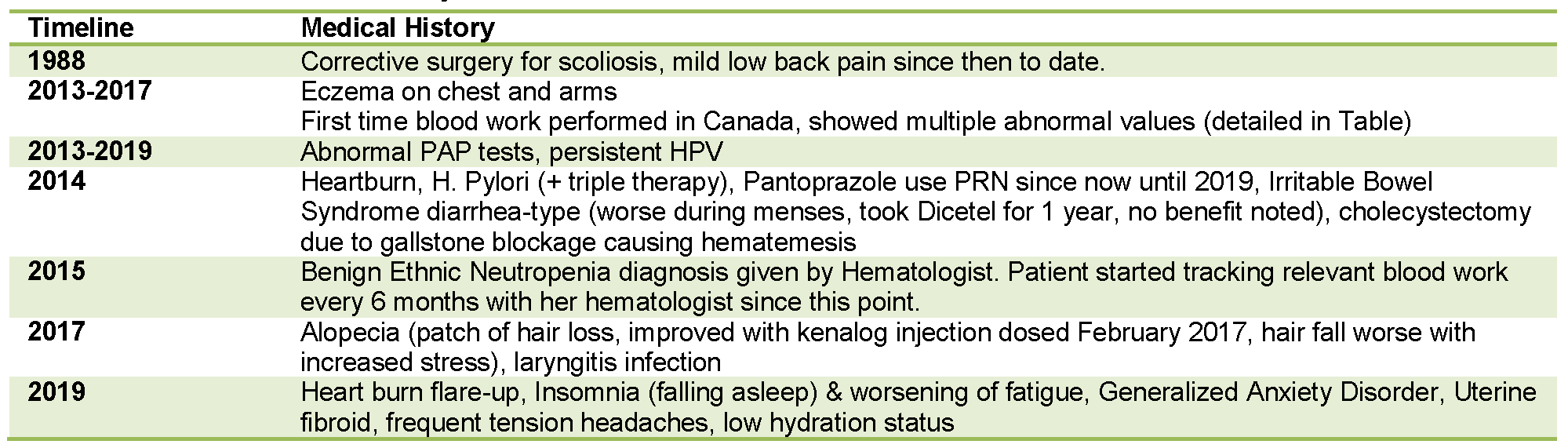
Figure 1. Relevant medical history: Timeline of relevant medical history for the patient discussed in this case report.
Pertinent negatives include absence of allergies, fatigue (patient rated her energy at a 7/10, 10= high energy), fever, vomiting, edema, changes in appetite, bleeding, weight loss, hepatomegaly and jaundice. Patient was not using any illicit drug or herbal treatment prior to their illness presentation. Patient received a negative score on the heavy metal toxicity screening questionnaire performed in November 2019. The patient’s only personal food restrictions include avoidance of pork and seafood. She did report food sensitivities to spicy food, causing gastrointestinal upset and loose stools. Pertinent family history includes presence of vitiligo, arthritis, cancer, high blood pressure, hepatitis, kidney disease and osteoporosis.
Abnormal and borderline normal blood work measures are reported in Figure 6. This includes evidence of leukopenia (white blood cell count <4000 cell/uL), anemia (hemoglobin <115g/L), thrombocytopenia (platelet count <100,000 cells/uL), poikilocytosis, risk of anemia (low B12 and Iron), elevated gamma globulin, elevated erythrocyte sedimentation rate, elevated immunoglobulins and lowered alanine aminotransferase.
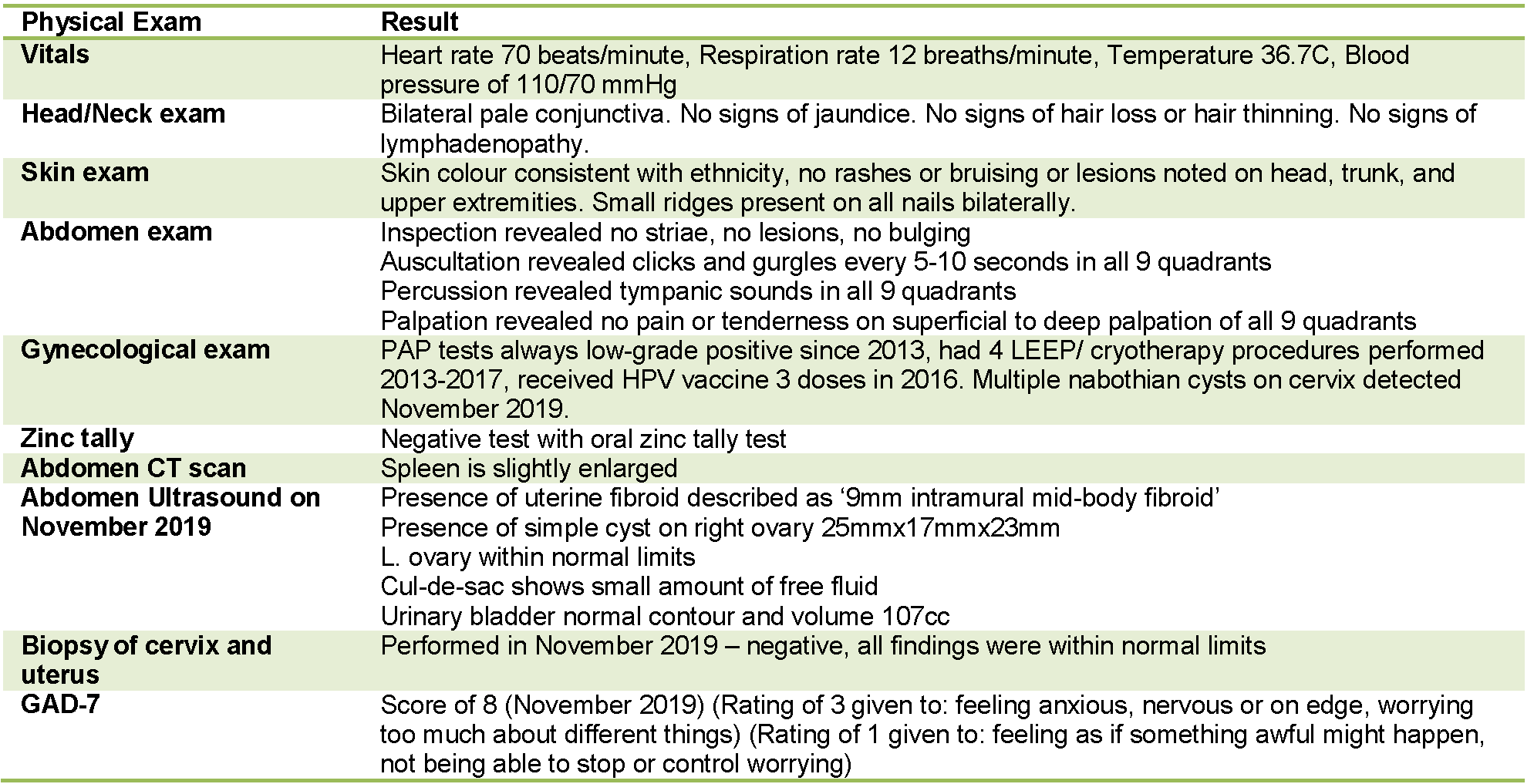
Figure 2. Relevant physical exams and investigations: Description of relevant objective findings for the patient discussed in this case report.
Patient appeared well-nourished, alert and oriented at all visits. Review of systems revealed mildly impacted energy levels (6-7/10, 10= high), trouble falling asleep insomnia, average sleep hours of 12AM-6AM, lightheaded when low food intake and when on period, frequent bilateral temporal-occipital tension headaches (rated 8/10 intensity, 10= high), occurrences of achy 8/10 (10= high intensity) pain on right flank region of abdomen that radiates to the ipsilateral back (symptom not recreated on abdomen exam, and was found to be muscular in origin due to workout routine), consistent normal bowel movements, nausea present sometimes in the morning, menses usually regular.
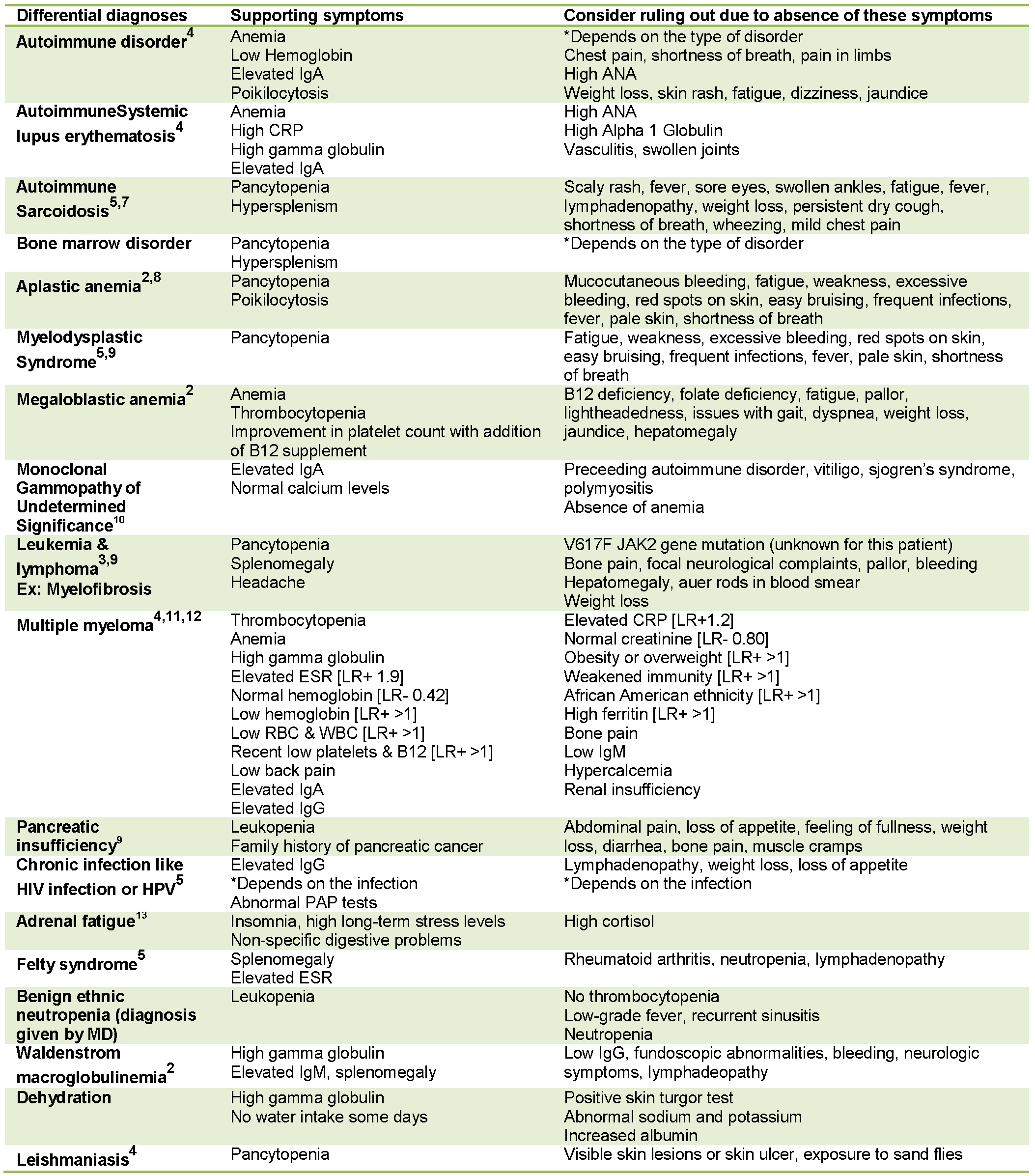
Figure 3. List of differential diagnoses: Description of various differential diagnoses and reasons for ruling them in or out for the patient discussed in this case report.
As reported above, all potential causes of pancytopenia were taken into account in the differential diagnoses. The patient has not been given a clear diagnosis from either of her healthcare specialists as of yet due to the improvements noted in certain blood markers detailed in Table 6. The patient received the diagnosis of an autoimmune disorder by her first hematologist. Potential primary diagnoses include an underlying nutritional deficiency overlapping with one of the differential diagnoses listed above.
Treatment Protocol
RA is following our RSNC treatment protocol of a structured diet and lifestyle plan, and supplement protocol to support her nutrient deficiencies determined by blood work. Some of the protocol targets include endocrine-balancing diet, nutrients depleted by long-term 40MG pantoprazole proton pump inhibitor use for heartburn. Nutrients depleted include B12, calcium, magnesium, zinc, folic acid, probiotics and iron [14]. Patient reported drinking 0-0.5L of water daily (includes all non-caffeinated, non-alcoholic beverages), therefore this was addressed as well.
With regards to her symptom of heartburn, we tracked and eliminated specific trigger foods and addressed including these foods in minimal amounts. Additionally, we addressed lifestyle factors that promote heartburn, such as eating too quickly and lying down immediately after eating. These changes along with acutely 500mg DGL-Licorice chewable orally before bed helped to eliminate her heartburn. Patient found that the magnesium supplementation helped her achieve a more restful sleep and benefit anxiety levels. Patient noted she noticed a benefit in hair growth and thickness while on the treatment protocol. Patient noticed a benefit to energy levels while on protocol. It is important to note that the patient is currently not taking any medications.
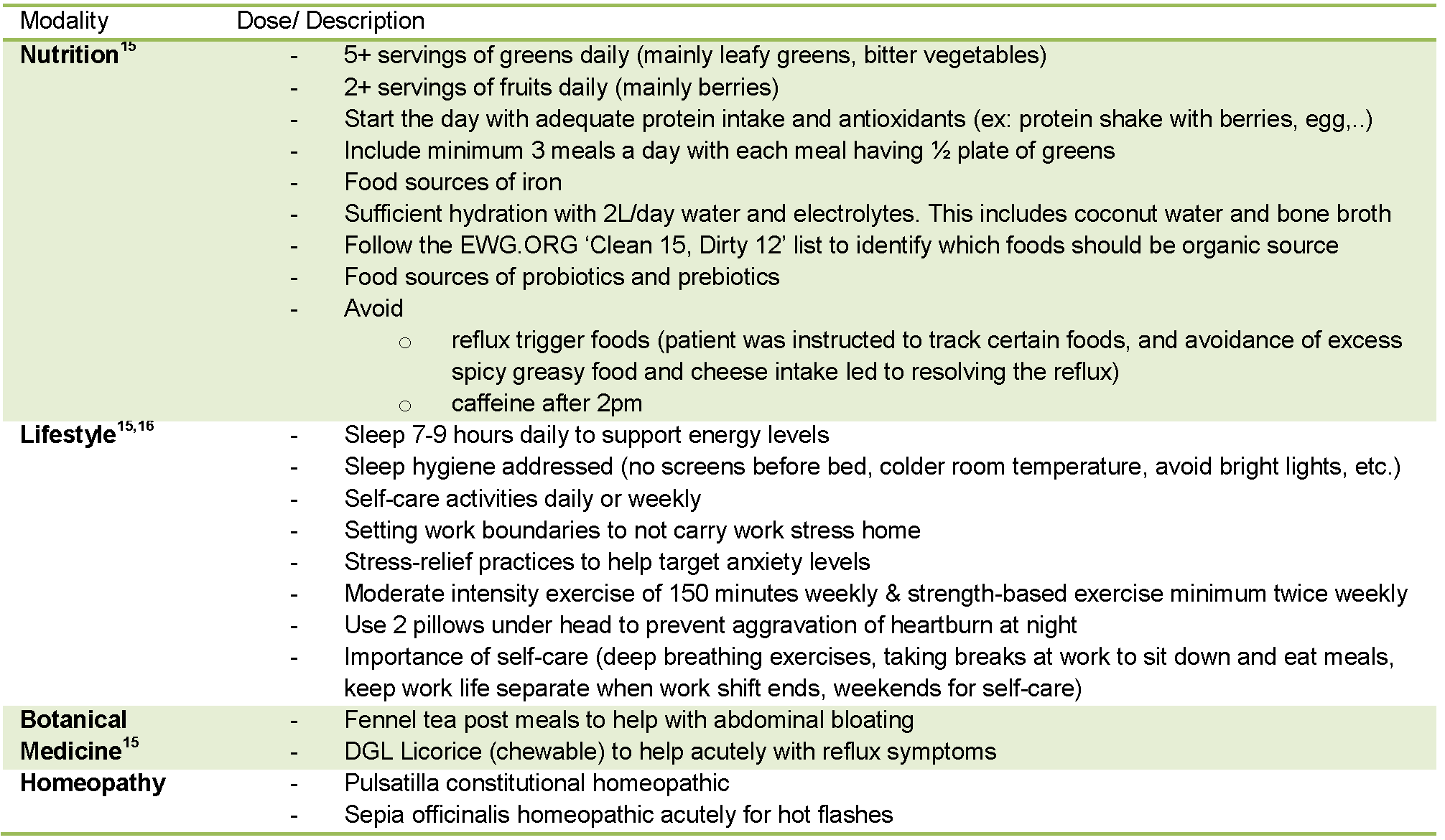
Figure 4. Treatment protocol Part-1 of 2 for the patient followed at RSNC: Description of treatment provided at RSNC separated by modalities used.
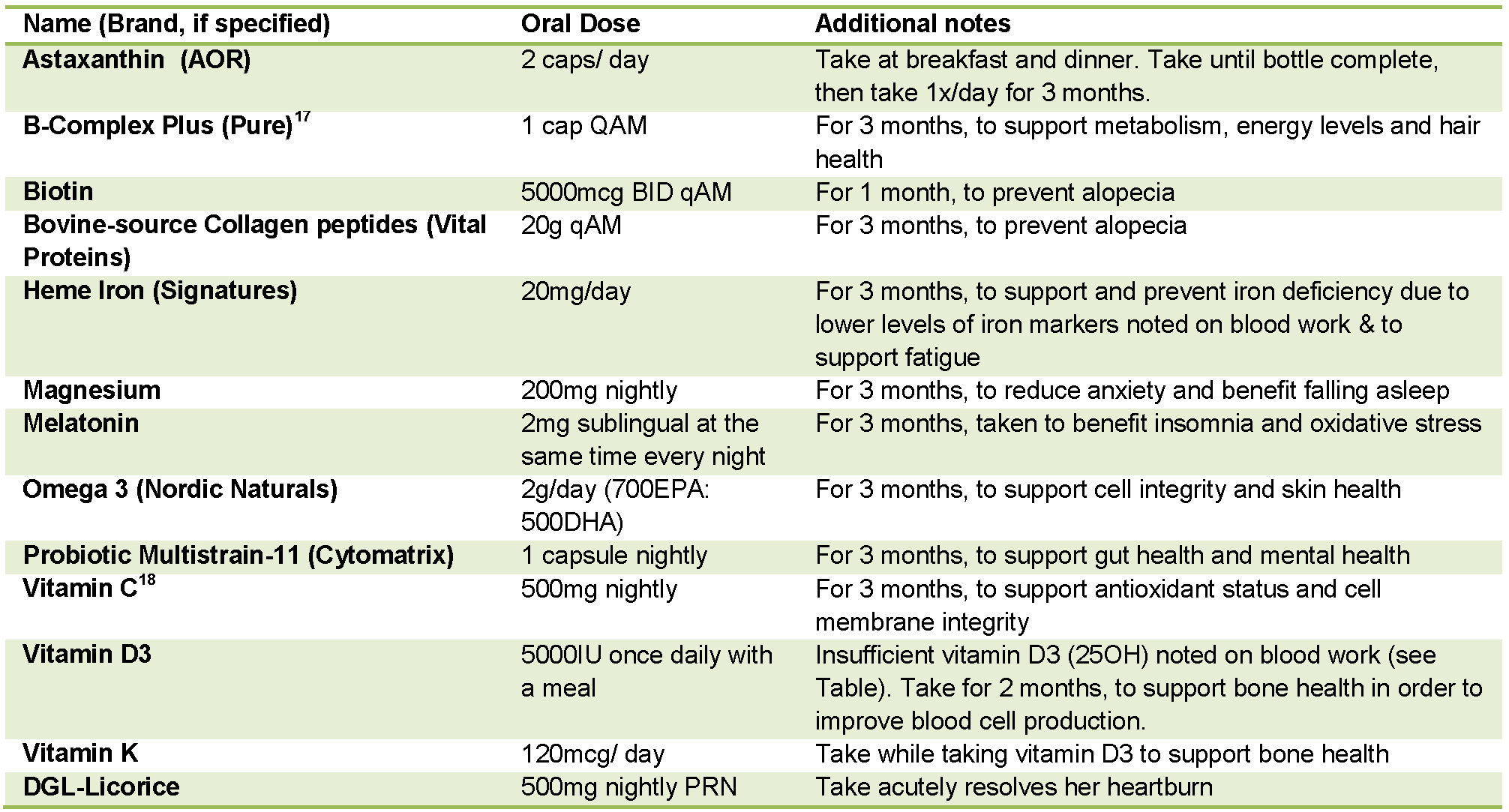
Figure 5. Treatment protocol Part-2 of 2 for the patient followed at RSNC: Description of natural health products used including doses and additional notes or instructions.
The patient was made aware of all costs associated with the supplement prescriptions, and she requested to have the best recommended products with no financial issues reported. Therefore, there was no impact of low cost influencing our protocol.
Outcomes
Patient blood reports from venipuncture, blood smear, and electrophoresis are included below in Table 6 to track progress of treatment protocol and patient health condition. Blood reports were the main outcome used as this was the patient’s priority and chief concern.
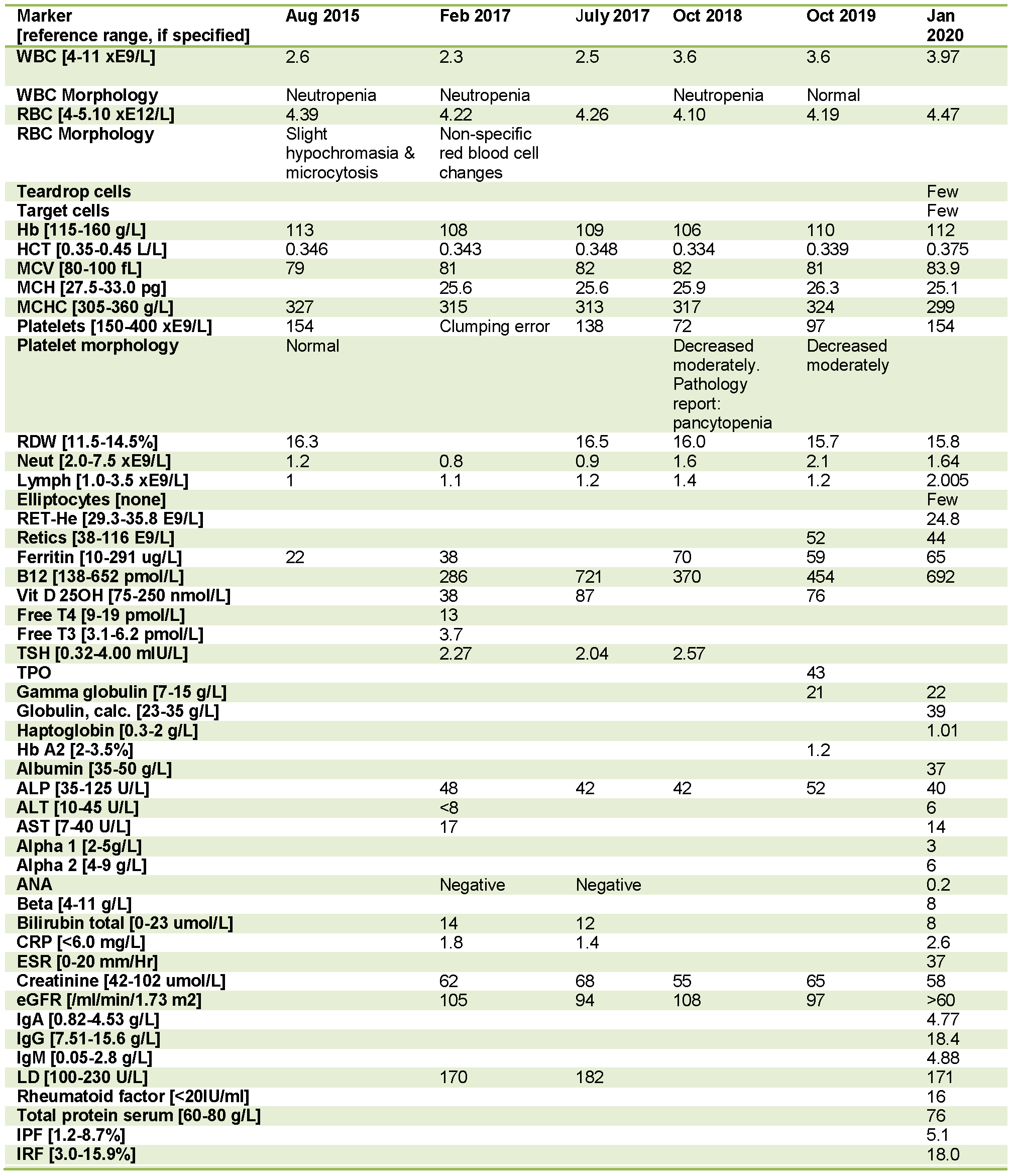
Figure 6. Analysis of blood values for the patient discussed in this report: This table includes abnormal and borderline normal blood work measures for RA from 2015-2020.
Discussion
This case report represents criteria #2 of the case report selection criteria – unexpected or unusual presentations of a disease. Based on history and physical exam, various dietary and lifestyle strategies overlapped with presenting signs and symptoms. For one example, initial lack of B12 rich foods in diet and initial lowered B12 levels on bloodwork. Based on therapeutic order of Naturopathic Medicine, a potential underlying unknown cause or probable correlation of nutrient deficiency for these symptoms was considered. The patient’s blood values and presenting concerns were seen to improve after starting a protocol of supplements to correct possible nutrient deficiencies based off her blood work, dietary intake and symptom presentation. Treatment protocol provided is summarized in Table 6. Treatment also included recommendations for a second hematologist opinion on blood work, based off case consult with Dr. O. Singh and Dr. M. Salsberg.
The two main broad scale diagnoses given to the patient by her hematologists include autoimmune disorder and benign ethnic neutropenia. Currently, there is no existing literature on naturopathic support for benign ethnic neutropenia. This case report will help build the research base for this presentation of condition and further the knowledge of naturopathic support in the treatment of various abnormal blood markers. Through this research, I hope to present insight into which blood markers respond to which naturopathic treatment options.
One limitation of this report is due to a risk benefit analysis, bone marrow examination was not recommended for this patient; therefore we are unable to determine true pathophysiology cause of her abnormal blood values. The patient continues to follow-up with her hematologist every 6 months, to monitor blood work and re-assess need for further testing and treatment. The patient reported signs of relief to find that she has been given some strategies within her control to help alleviate abnormalities in blood markers.
Conclusion
In conclusion, we learn the importance of the nutritional and lifestyle therapeutic modalities in reducing progression of this undetermined blood disorder. From this research we can reaffirm the importance of following therapeutic order and addressing basic nutrient requirements when addressing blood disorders. This report highlights the importance of addressing mental health for the patient with an undiagnosed health condition. The conclusion of this report highlights the importance of naturopathic medicine as supportive care in addressing all possible biopsychosocial determinants of the patient’s blood results while working on discovering the root etiology of blood disorders. The goal of this report is to broaden resources of the medical community to advance our knowledge on etiologies of various blood disorders and improve strategies on effective diagnosis and management of blood disorders. Larger scale clinical trials on this topic are required to establish efficient guidelines for determining etiology and appropriate management of early presentations of hematological disorders. This research will aid in understanding disease processes that can affect various blood markers and contribute to efficient care provided to patients with abnormal values detected on blood work.
Patient’s Perspective
Prior to her parent’s fatal health diagnoses, the patient reported she did not quite understand the meaning of taking care of her health. After blood work in 2015 showed multiple abnormal values, the patient tried to focus more on her health as a priority. However, due to family health reasons and personal work-life situation, the patient fell off-track of prioritizing herself and her health multiple times. The patient expressed her anxiety around her health due to the passing away of both of her parents within the last 7 years. The patient’s hematologist opinions advised the patient against all worries about her health, and all other health care providers supported their expert opinions. However, the patient reports she does not feel like everything is okay with regards to her health. She does not want to contradict expert opinions and the patient stated sometimes she feels like “it’s all in [her] head”. Her goals at the RSNC are to follow her health reports with her, provide guidance and provide any naturopathic support to help improve her health status. She was grateful and appreciative of the ability to converse about her health situation confidentially with Naturopathic Medicine. She found that relieving her anxiety by talking about her health and supplementing certain products helped her feel better. This benefit was reflected on her blood work. Currently, she would like to work together with her healthcare providers as a health team to figure out what would be the best protocol for her to improve her health. She appreciates getting her health questions answered and this guidance improves her feelings of anxiety about her health.
Competing Interests
The author declares that they have no competing interests.
Authors’ Contributions
MD analyzed, interpreted the patient data, and wrote this final manuscript with respect to this case.
Acknowledgements
Acknowledgement to Dr. Onkar Singh, ND, from the Canadian College of Naturopathic Medicine for his role as clinic supervisor in management of this case and to Dr. Joy Dertinger, ND, for her role as the case advisor in her guidance and support on this report. Acknowledgement also to Dr. M. Salsberg for his opinions provided at a case consult session.
References
[1] Canadian Cancer Society (2016). Blood cancer in canada facts & stats. Toronto.
[2] Dasgupta S, Mandal PK, & Chakrabarti S (2015). Etiology of Pancytopenia: An Observation from a Referral Medical Institution of Eastern Region of India. J Lab Physicians , 7 (2), 90-95.
[3] Jalaeikhoo H, Kashfi SM, Azimzadeh P, Narimani A, Moghadam KG, Rajaienejad M, Ariana M, & Keyhani M. (2017). Acute Myeloid Leukemia as the Main Cause of Pancytopenia in Iranian Population. Iran J Pathol , 12 (3), 265-271.
[4] Gudina EK, Amare H, Benti K, Ibrahim S, & Mekonnen G. (2018). Pancytopenia of Unknown Cause in Adult Patients Admitted to a Tertiary Hospital in Ethiopia: Case series. Ethiop J Health Sci , 28 (4), 375-382.
[5] Yokus O, & Gedik H. (2016). Etiological causes of pancytopenia: A report of 137 cases. Avicenna J Med , 6 (4), 109-112.
[6] Carere RP, & Clemes IL. (1962). An unusual cause of splenomegaly and pancytopenia (secondary hypersplenism). Canad. Med. Ass. J. , 86, 833-835.
[7] Akinsanya L, Hussain I, Awoniyi D, & Usman K. (2008). Leucopenia as Presentation of Sarcoidosis. Int J Health Sci (Qassim) , 2 (1), 109-112.
[8] Biswajit H, Pratim PP, Kumar ST, Shilpi S, Krishna GB, & Aditi A. (2012). Aplastic Anemia: A Common Hematological Abnormality Among Peripheral Pancytopenia. N Am J Med Sci , 4 (9), 384-388.
[9] Weinzierl EP, & Arber DA. (2013). The Differential Diagnosis and Bone Marrow Evaluation of New-Onset Pancytopenia. American Journal of Clinical Pathology , 139 (1), 9-29.
[10] Shimanovsky A, Alvarez AJ, Murali S, & Dasanu CA. (2016). Autoimmune manifestations in patients with multiple myeloma andmonoclonal gammopathy of undetermined significance. BBA Clinical , 12-18.
[11] Sridevi HB, Rai S, Suresh PK, Somesh MS, & Minal J (2015). Pancytopenia in Multiple Myeloma- An Enigma: Our Experience from Tertiary Care Hospital. J Clin Diagn Res , 9 (11), EC04-EC06.
[12] Koshiaris, C. V. (2018). Early detection of multiple myeloma in primary care using blood tests: a case-control study in primary care. British Journal of General Practice , 68 (674), e586-e593.
[13] Shaaban H, Modi T, Modi Y, & Sidhom IW. (2013). Hematologic Recovery of Pancytopenia after Treatment of Hashimoto’s Thyroiditis and Primary Adrenal Insufficiency. N Am J Med Sci , 5 (3), 253-254.
[14] Heidelbaugh, J. (2013). Proton pump inhibitors and risk of vitamin and mineral deficiency: evidence and clinical implications. Ther Adv Drug Saf , 4 (3), 125-133.
[15] Yeh AM, & Golianu B. (2014). Integrative Treatment of Reflux and Functional Dyspepsia in Children. Children (Basel) , 119-133.
[16] Aylett E, Small N, & Bower P. (2018). Exercise in the treatment of clinical anxiety in general practice – a systematic review and meta-analysis. BMC Health Serv Res , 18, 559.
[17] Kim M, Lee SE, Park J, Lim J, Cho BS, Kim YJ, Kim HJ, Lee S, Min CK, Kim Y, & Cho SG (2011). Vitamin B(12)-responsive pancytopenia mimicking myelodysplastic syndrome. Acta Haematol , 125 (4), 198-201.
[18] Lal A, Mishra AK, Sahu KK, & Noreldin M. (2019). Scurvy of modern age: Rare presentation with pancytopenia. Blood Cells, Molecules, and Diseases , 77, 76-77.


